Episode 8 (iTunes or Listen Here)
The Free Open Access Medical education (FOAM)
This week we review Dr. David Story’s talk from SMACC GOLD, “Is Chloride a Poison?” Dr. Story discusses the Stewart ion approach to acid-base, driven by the independent variable, the Strong Ion Difference (SID), which is the difference between the sums of concentrations of the strong cations and strong ions (typically Sodium and Chloride). He also reviews literature that suggests that there may be morbidity and even mortality associated with large volume infusions of 0.9% NaCl (NS), although more research is required in this arena to determine the patient oriented sequelae. Perhaps we should be using more balanced solutions such as lactated ringers (LR).
Also, SMACC is awesome, listen to the talks from SMACC GOLD and come meet us in Chicago next June!
Literature on the topic:
Other FOAM Acid-Base Resources:
- EMCrit’s Acid-Base: Part I, II, III, IV
- ScanCrit – Stewart’s Acid Trip
The Bread and Butter
We summarize some key topics from the following readings, Tintinalli (7e) Chapters 19,21; Rosen’s (3e) Chapters 124, 125 …but, the point isn’t to just take our word for it. Go enrich your fundamental understanding yourself!
IV Fluids – Know the Composition (PV card from ALiEM)
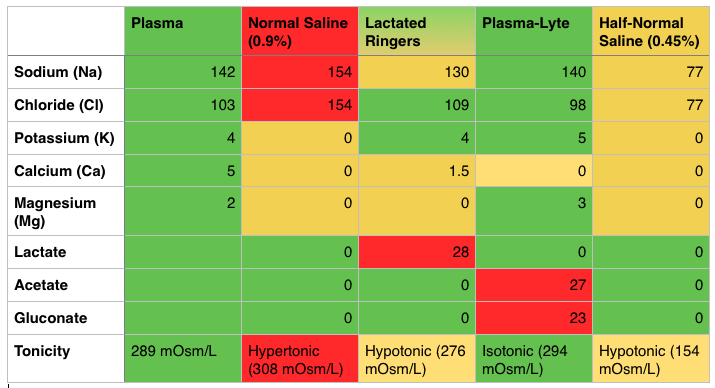
Costs – NS (0.9%) is the cheapest, coming in at just over a US dollar per Liter and LR is slightly more expensive (most estimates are approximately $0.50 more per liter). Plasma-lyte is more expensive, costing several dollars more per liter.
Downsides of Normal Saline (NS, 0.9%)
- Hypertonic, hypernatremic, hyperchloremic – it has a little too much of everything and is acidic, with a pH of 5.0 [1]
- The SID (Strong Ion Difference) of NS is 0, far less than the physiologic or normal SID of 38. This is where the non-anion gap acidosis comes into play [1].
Caution with Lactated Ringers (LR)
- LR contains calcium and some labs studies have shown that this may cause clotting; thus, major societies say LR is incompatible with blood products. There are some studies to show that this may not be as big of a deal as previously thought: Albert et al, Cull et al, Lorenzo et al.
- May interfere with Lactate clearance -A study of healthy individuals demonstrated that LR did not affect serum lactate levels [2]. However, often we are doing these large volume resuscitations in the critically ill who may have hepatic insufficiency and, thereby, reduced lactate clearance. There is worry that LR may increase the serum lactate, making it difficult to gauge resuscitation by lactate clearance. Paul Marino’s ICU Book states that significant skewing of the lactate is unlikely unless the patient’s ability to hepatically clear lactate is nil and the patient has gotten several liters of LR [1].
FOAM Resources:
- Boring EM – Normal Saline – The Coke of Crystalloid Fluids
Hyponatremia – Na+ <135 mEq/L
Symptoms: often asymptomatic but may see vague symptoms such as nausea, vomiting, myalgias, lethargy. Values <120 mEq more associated with symptoms and <113 mEq, may see seizures/coma.
Causes:
- Hypovolemic – Extra-renal: dehydration (vomiting, diarrhea, small bowel obstruction, burns), infusion of hypotonic fluids, Renal: thiazide diuretics, Renal Tubular Acidosis, osmotic diuresis, aldosterone/mineralocorticoid deficiency
- Euvolemic – SIADH (syndrome of inappropriate secretion of antidiuretic hormone), water intoxication, drugs (NSAIDs, APAP, TCAs, sulfonylureas, morphine, carbamazepine, etc), beer potomania
- Hypervolemic – think organ failure and people who are third spacing fluids. Congestive Heart Failure, Liver Failure, Renal Failure
Other FOAM Hyponatremia Resources:
Generously donated Rosh Review questions (scroll for answers)
Question 1.[polldaddy poll=8191357]
Question 2. A 23-year-old woman presents with seizures. The patient received 2 mg of lorazepam by EMS but continues to seize. Serum lab tests show the following: sodium 118, potassium 3.6, chloride 90, bicarbonate 21, BUN/Cr 10/1.0, glucose 89. [polldaddy poll=8191360]
Additional References:
1.Tizard, H. Chapter 12: Colloid and Crystalloid Resuscitation. Marino’s The ICU Book, ed 4.Lippincott Williams & Wilkins, 2007.
2.Didwania A, Miller J, Kassel D, Jet al. Effect of intravenous lactated Ringer’s solution infusion on the circulating lactate concentration: Part 3. Results of a prospective, randomized, double-blind, placebo-controlled trial.Crit Care Med. 1997 Nov;25(11):1851-4.
Answers.
1.C -The syndrome of inappropriate secretion of ADH (SIADH) is defined by the secretion of ADH in the absence of an appropriate physiologic stimulus. Its hallmark is an inappropriately concentrated urine, despite the presence of a low serum osmolality and a normal circulating blood volume. Causes of SIADH include central nervous system disorders, pulmonary disease, drugs, stress, pain, and surgery. Therefore, the above patient, with a known history of lung cancer and hyponatremia, most likely has SIADH and exhibits the following lab findings: serum osmolarity low, urine osmolarity high, urine sodium high. Psychogenic polydipsia (D) is a rare cause of euvolemic hyponatremia and is seen in psychiatric patients who consume large amounts of free water (in excess of 1 L/hr). This large consumption overwhelms the kidney’s ability to excrete free water. Patients will exhibit serum osmolarity low, urine osmolarity low, urine sodium low. Diabetes insipidus (B) results in the loss of large amounts of dilute urine from the loss of concentrating ability in the distal nephron. This may be due to a central cause—such as the lack of ADH secretion from the pituitary—or a nephrogenic cause—such as the lack of responsiveness to circulating ADH. Laboratory workup that invariably shows serum osmolarity high, urine osmolarity high, urine sodium low (A) rarely occurs.
2.A-This patient presents with prolonged seizure activity and hyponatremia and should emergently be treated withhypertonic saline. Hyponatremia is defined as a serum sodium level <135 mEq/L and is the second most common electrolyte abnormality after hypokalemia. The symptoms and signs of hyponatremia depend on the patient’s volume status, the cause and the rapidity of the change in serum sodium. Typically, patients with acute changes will have more severe symptoms including nausea, vomiting, confusion, stupor and seizures. Chronic hyponatremia will typically present with mild neurologic symptoms as well as lower serum sodium levels than acute hyponatremia. In patients without neurologic symptoms, volume status should be assessed and additional labs should be sent off to determine the cause of hyponatremia (urine sodium, osmolarity etc.). Patients with neurologic symptoms should be aggressively treated with 3% hypertonic saline. When correcting serum sodium, it is important to increase the serum sodium by no more than 0.5 mEq/L/hour and by no more than 10 – 12 mEq/day. More rapid changes can lead to central pontine myelinolysis, a crippling neurologic disease.