(iTunes or listen here)
The Free Open Access Medical Education (FOAM)
This week we review EM in 5’s episode on the Neuro Exam of the Hand.
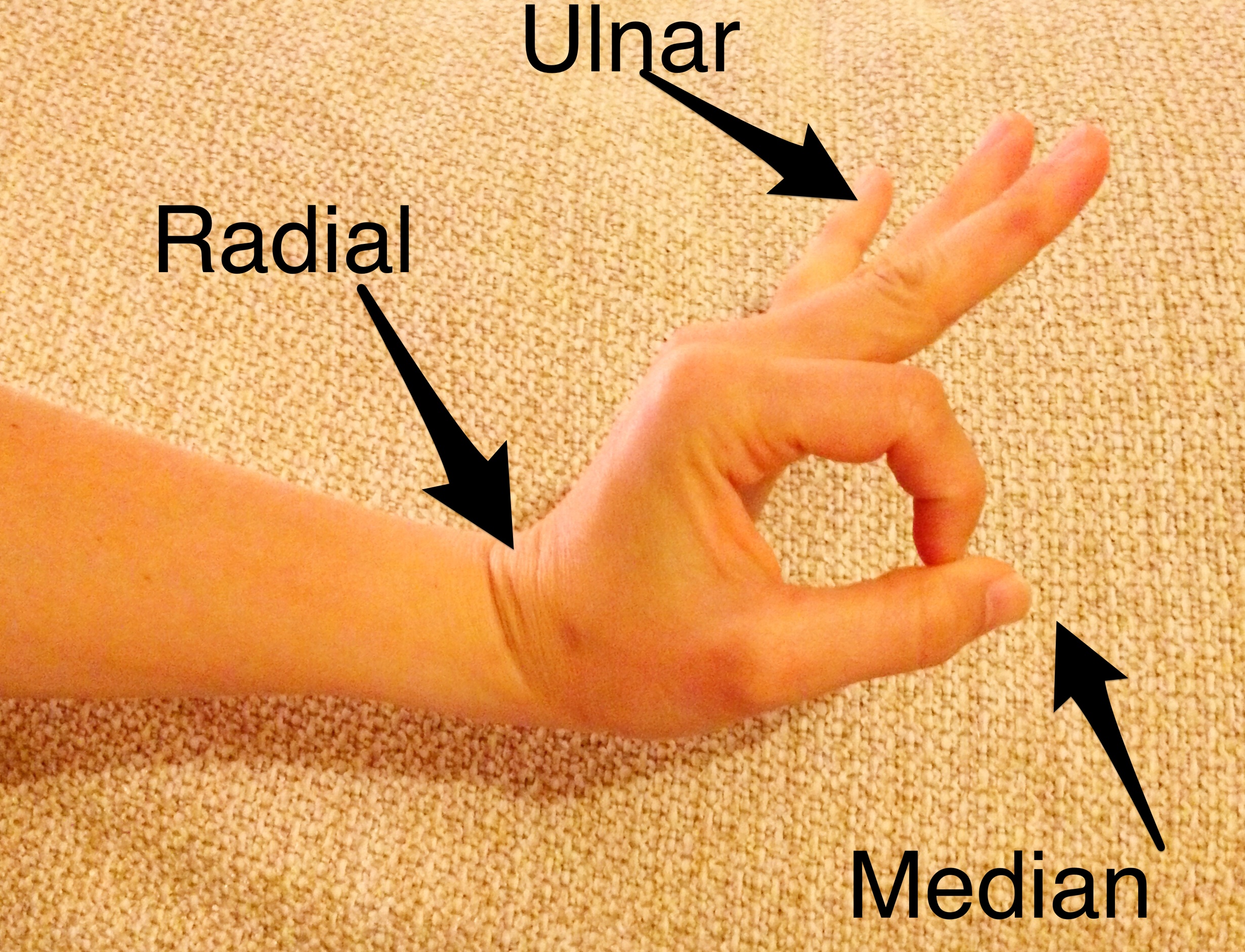
All 3 motor nerves (median, ulnar, radial) in one motion:
- Make the “ok sign” and try to break the ring formed by the thumb and index finger – median
- Memory aid: The median is “ok.”
- Spread 3-5 fingers apart and adduct against resistance – ulnar
- Memory aid: The intertriginous areas between abducted fingers make a “U” for ulnar
- Dorsiflex wrist – radial
- Memory aid…if you look really hard, the the dorsiflexed hand and arm appear to be a sideways, lower case “r”
…all in one
The Bread and Butter
We summarize some key topics from the following readings, Tintinalli (7e) Chapter 280, 295 ; Rosen’s 8(e) Chapter 50 – a well written chapter, but, the point isn’t to just take our word for it. Go enrich your fundamental understanding yourself!
Flexor Tenosynovitis
Kanavel’s Cardinal Signs (look for words that start with “F”).
- Pain on passive extension -happens early
- Finger held in flexion – see above point..extension hurts!
- Fusiform (uniform) swelling of finger – most common
- Tenderness along flexor tendon sheath – happens later [3]
Treatment – serious surgical emergency and failure to treat adequately can result in necrosis, proximal spread, and loss of use of hand.
- IV Antibiotics – penicillinase resistant penicillin (ampicillin-sulbactam, piperacillin-tazobactam) + vancomycin (if suspect MRSA)
- Consult hand surgery
- Admit
Hand Pearls
Mallet Finger: Disruption of the distal extensor tendons, often caused by a jamming injury, hyperextension, or crush. Look for bruising at the distal interphalangeal joint. Closed injury – immobilization. Open- extensor tendon repair.
High pressure injection injuries (paint gun, on the job stuff): Worse than they look. Tetanus, IV antibiotics, consult hand.
Digit amputation storage: Cover the stump with saline gauze and wrap amputated digit in saline soaked gauze. Put the saline soaked gauze covered digit in airtight plastic bag and place that bag in a bag on ice.
Amputations have best success of reimplantation if they are:
- Clean cut (saw, etc) versus a crush injury
- Distal (distal finger > proximal finger > hand)
Learn to Splint Like a Pro (via ERCast) and document a thorough neurovascular exam pre and post-splinting.
Bonus Rosenalli Myth Buster: Common teaching prevails that epinephrine should not be used with anesthesia of the fingers, nose, toes, penis, etc. FOAM has debunked this (SMART EM podcast), as well as peer reviewed literature: Waterbrook et al, Truth, and epinephrine, at our fingertips: unveiling the pseudoaxioms.
- Use of epinephrine in finger, nose, etc IS Rosenalli approved [Ch 40, Tintinalli 7e; Ch 3 Rosen’s 8e].
Generously Donated Rosh Review Questions (Scroll for Answers)
Question 1. Which of the following is classically seen in flexor tenosynovitis?
A. Extended position of the involved digit
B. Fusiform swelling of the digit
C. Tenderness over the extensor sheath
D. Vesicular eruption over the flexor surface
Question 2. A 42-year-old man presents to the ED with an amputation of his left thumb just proximal to the interphalangeal joint. The injury occurred 1 hour ago at a rural construction site while the patient was operating a power miter saw. The thumb is brought in, in a sandwich bag, along with the patient. Which of the following is true regarding predictors of successful replantation?
A. Crush injuries have a high success rate of replantation
B. Digits have better tolerance for ischemia than limbs have
C. The amputated part should be kept cold and dry
D. The patient’s social history adds little value to the success rate of replantation
References
1. Chapters 3, 50. Rosen’s Emergency Medicine, 8e.
2.Chapters 40, 280, 295. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 7e. New York, NY: McGraw-Hill; 2011
3. Draeger RW, Bynum DK Jr. Flexor tendon sheath infections of the hand. J Am Acad Orthop Surg. 2012 Jun;20(6):373-82. doi: 10.5435/JAAOS-20-06-373.
Answers.
1. B. The flexor tendons of the fingers are covered by a double layer of synovium to promote gliding of the tendon underneath. Infections in the synovial spaces in the hand tend to spread along the course of the flexor tendon sheaths and may extend proximally to the hand. Infections are usually due to penetrating trauma involving the sheath but occasionally from hematogenous spread. Four cardinal signs of acute flexor tenosynovitis are usually present to help distinguish tenosynovitis from other hand infections. These criteria are referred to as the Kanavel’s signs. Flexor tenosynovitis is a surgical emergency. Consultation with a hand surgeon is warranted along with intravenous antibiotics. The affected digit is held in a flexed (A), not extended, posture. The tenderness is over the flexor (C) sheath, not extensor. Vesicles (D) are not commonly associated with flexor tenosynovitis. A localized herpes simplex infection may cause vesicles to form on a digit
2. B. Ischemia time is one of the most important predictors of successful replantation. Digits have less muscle mass to oxygenate and tolerate ischemia better than amputations more proximally along the limb. Replantation of limbs must be completed within 4–6 hours, but digits can tolerate an ischemic time of up to 8 hours, given proper preservation. Crush injuries (A) have a low success rate for replantation due to the significant destruction of neurovascular structures. The amputated body part should be irrigated with normal saline to remove gross contamination, wrapped insterile gauze moistened with saline (C), and placed in a sterile, watertight container. This container should be placed in ice water, but the digit itself should not be submerged. Research has repeatedly shown that tobacco use (D), especially smoking after surgery, will worsen the chance of successful replantation. Obtaining a social history is important in these cases.