(ITUNES OR LISTEN HERE)
The Free Open Access Medical Education (FOAM)
We cover an EMcrit episode on Semantics of End of Life Discussions with Dr. Ashley Shreves as well as pearls from another favorite episode with her, Episode 93 – Critical Care Palliation. We can’t do these episodes justice summarizing them so listen to them. (Update: Apparently these podcasts were taken down due to personal reasons. From what we understand you may be able to obtain a copy by contacting the EMcrit site).
Screen who to have “the conversation” with looking for patients with signs of instability:
- 85 y/o and older
- dementia/frailty
- advanced cancer/disease
Key conversational points:
- Lead with, ” I’m so worried about (the patient).”
- “What do you think your (mom/dad/etc) would say about how she is now?”
- “Got it.” Whether a family member agrees or disagree, let them know you heard them.
If a patient/family member are overly optimistic about the patient getting better one can try, “Many people find it helpful to talk about what would we should do if (the patient) doesn’t get better.”
Respect patient/family values that differ from yours. If the patient’s family just wants the heart beating regardless, and that’s ok. Per Dr. Shreves, this population is 5-10% and may be called “vitalists.”
Another key point Dr. Shreves emphasizes is that palliative care, comfort care, and allowing a natural death often mean escalating care – ensuring the patient is comfortable, clean, etc.
Core content
We delve into core content on vertigo using Rosen’s Medicine (8e) electronic chapter, “End of Life,” and Tintinalli’s Emergency Medicine: A Comprehensive Study Guide (7e) Chapter 297 “Death and Dying.”
DNAR (Do Not Attempt Resuscitation) – technically only speak to a patient’s wishes to receive CPR [3]. Problematic for several reasons, including:
- Issue lies in the word “resuscitate,” which may be used to include fluids, antibiotics, vasopressors, advanced means of ventilation or, at the extreme, CPR. The AHA guidelines have moved to DNAR from DNR but even this language isn’t clear.
- Major societies are moving towards the language AND, Allow Natural Death [4].
- AND is preferred because it describes what happens and is more clear, is kinder language laden with reduced guilt
- The TRIAD II-IV studies surveyed EMS personnel, physicians, and medical students respectively and provided the participants with an advance care directive as well as case scenarios. The participants then indicated whether a patient was a DNR or full code and the appropriate action. Both physicians and EMS providers performed poorly and variably, indicating that the directives were not clear [5-7].
Palliative care and hospice are not interchangeable. Palliative care has a more broad definition and
- Palliative care: “An approach that improves quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual ” [1]. There is no time limit in this scenario.
- Hospice care: subset of patients that a doctor has estimated likely has 6 months or less to live [1].
Opioid Equivalents
Many terminally ill patients or those at the end of their life are on chronic opioids. While the opioid epidemic is a problem, this is not the appropriate population from which we should withhold appropriate analgesia. It can be difficult to convert between dosages to adequately treat a patient’s pain. Here’s a free calculator. 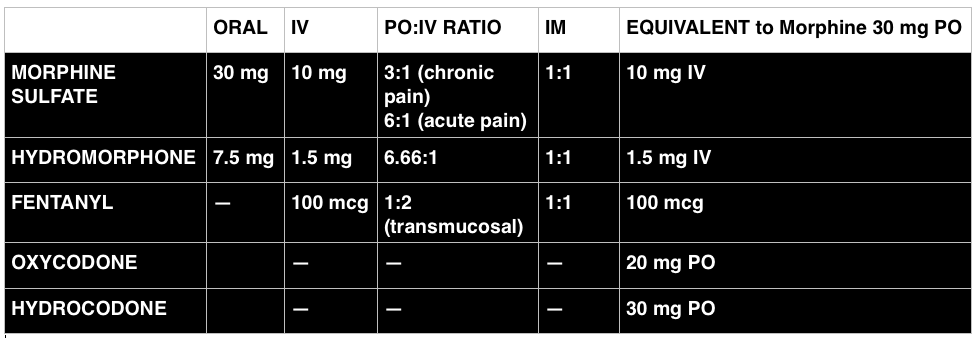
References
- Online Chapter. End of Life. In: Marx JA, Hockberger RS, Walls RM eds. Rosen’s Emergency Medicine, 8th e.
- Chapter 297. Death and Dying. In: Tintinalli JE, Stapczynski J, Ma O, Cline DM, Cydulka RK, Meckler GD, T. eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 7e. New York, NY: McGraw-Hill; 2011.
- Dugdale DC. .Do Not Resuscitate Orders.” MedlinePlus Medical Encyclopedia.
- Breault JL. DNR, DNAR, or AND? Is Language Important? Ochsner J. 2011;11(4):302
- Mirarchi FL, Kalantzis S, Hunter D, McCracken E, Kisiel T. TRIAD II: do living wills have an impact on pre-hospital lifesaving care? J Emerg Med. 2009;36(2):105–15. doi:10.1016/j.jemermed.2008.10.003.
- Mirarchi FL, Costello E, Puller J, Cooney T, Kottkamp N. TRIAD III: nationwide assessment of living wills and do not resuscitate orders. J Emerg Med. 2012;42(5):511–20. doi:10.1016/j.jemermed.2011.07.015.
- Mirarchi FL, Ray M, Cooney T. TRIAD IV: Nationwide Survey of Medical Students’ Understanding of Living Wills and DNR Orders. J Patient Saf. 2014 Feb 27.
- Gurwitz JH, Lessard DM, Bedell SE, Gore JM. Do-Not-Resuscitate Orders in Patients Hospitalized With Acute Myocardial Infarction. 2014;164.
- Adams DH, Snedden DP. How misconceptions among elderly patients regarding survival outcomes of inpatient cardiopulmonary resuscitation affect do-not-resuscitate orders. J Am Osteopath Assoc. 2006;106(7):402–4.
I can’t seem to find Dr. Weingart’s podcast with Dr. Shreves on the website or iTunes.
From what we’ve heard, these unfortunately had to be taken down due to personal reasons. I believe you can email at the emcrit site to get an emailed copy.