(ITUNES OR LISTEN HERE)
The Free Open Access Medical Education (FOAM)
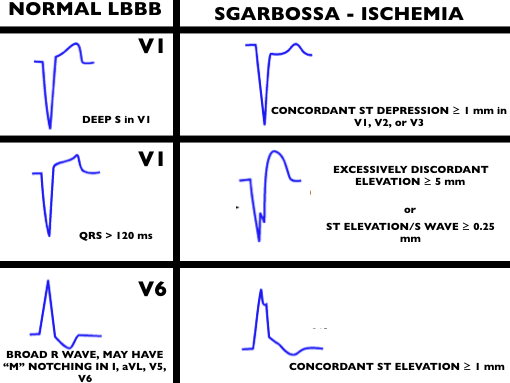
We cover a post from Dr. Smith’s ECG blog investigating ways to read ischemia on a ventricular paced ECG. In A Patient with Ischemic symptoms and a Biventricular Pacemaker, Dr. Smith asserts that the modified Sgarbossa criteria may work in ventricular paced rhythms as well as Left Bundle Branch Blocks (LBBB).
Core Content
We delve into core content on implantable cardiac devices using Rosen’s (8th edition), Chapter 80 and Tintinalli (8th edition)
Generously Donated Rosh Review Questions
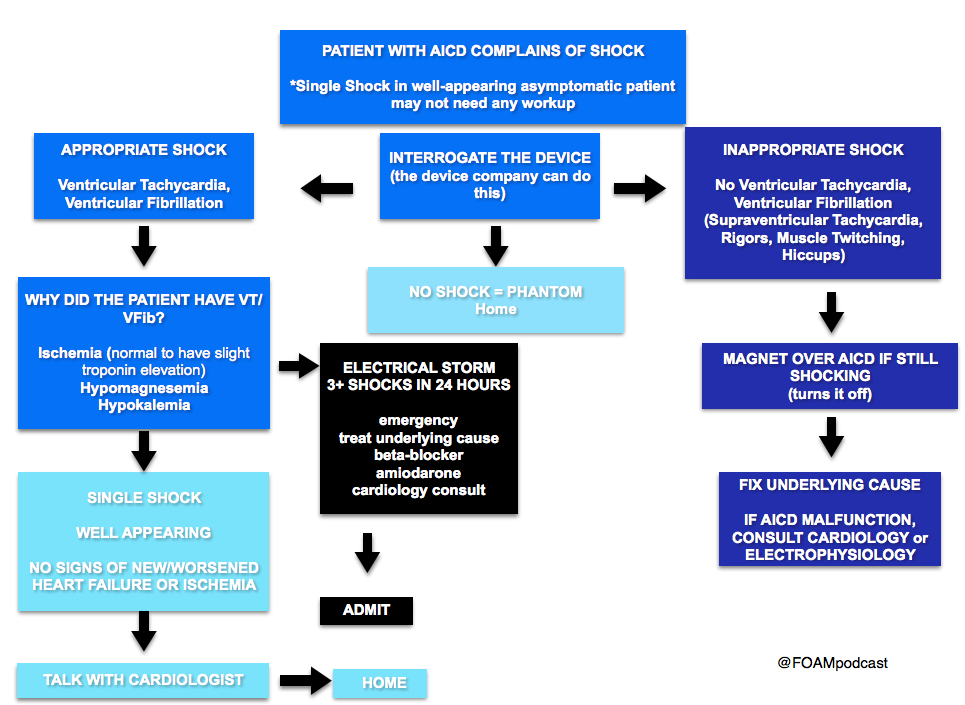
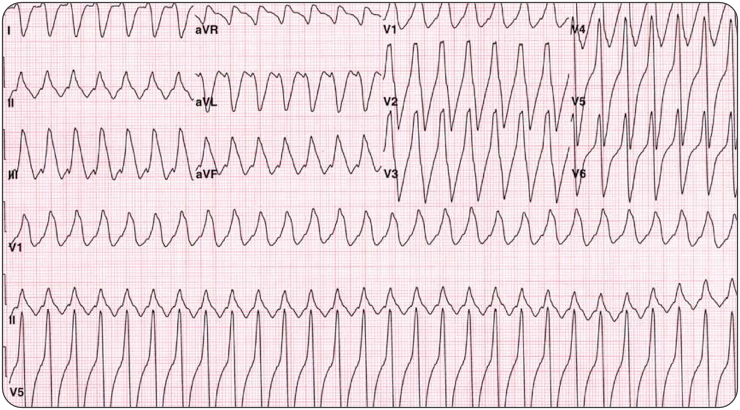
Question 1. A 44-year-old man with an automatic implantable cardioverter-defibrillator (AICD) in place presents with weakness and palpitations. Vitals are HR 180, BP 83/53, RR 28. His ECG is shown below. [polldaddy poll=9378494]
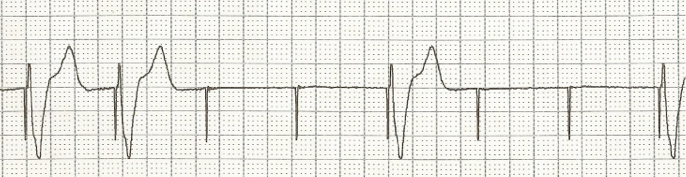
Question 2. A 76-year-old woman presents to the Emergency Department with generalized weakness and fatigue. She had a pacemaker placed one month ago. [polldaddy poll=9378495]
Answers
- Electrical cardioversion. This patient presents with unstable ventricular tachycardia and should immediately be electrically cardioverted. AICDs are placed for a number of indications but the goal is the treatment of ventricular dysrhythmias, particularly ventricular tachycardia (VT) and ventricular fibrillation (VFib). All AICDs have a right ventricular lead that is used for sensing. During insertion, the cardiologist determines the parameters for the device to deliver a shock. Despite the presence of these devices, patients may still present in ventricular dysrhythmias that have not been shocked if the device is malfunctioning. Patients may also experience inappropriate shocks. Regardless of the presence of the device, if a patient presents in an unstable dysrhythmia,electrical cardioversion or defibrillation (depending on the circumstance) should still be performed. This patient presents with ventricular tachycardia and hypotension and device failure. It is recommended that if a shock is to be delivered in a patient with an AICD that the pads not be placed over the device site. Otherwise, the presence of a device is not a contraindication to external electrical cardioversion/defibrillation.
Amiodarone (A) and procainamide (D) are antidysrhythmic agents that can be used in the treatment of stable ventricular tachycardia. Placing a magnet over the AICD site (C) may be beneficial in treating patients who are receiving inappropriate shocks. - A. Failure to capture can range from complete absence of pacemaker activity to pacemaker spikes being seen but not resulting in depolarization of the myocardium. Complete absence of activity can be due to battery depletion, fracture of the pacemaker lead (which is uncommon with today’s technology) or disconnection of the lead from the generator. Intermittent failure to capture is commonly due to lead displacement and is most likely to happen within the first month of placement. Failure to pace can also be due to impaired endocardium, which despite an intact and normally functioning pacemaker, will not depolarize properly. Causes include ischemia or infarction, hyperkalemia or use of class III antiarrhythmic drugs. Overpacing (B) can occur when atrial flutter develops during dual chamber pacing. The pacemaker may sense the atrial flutter waves resulting in a rapidly paced ventricular rate. A “runaway pacemaker”, a pacemaker that causes extreme increases in pacing rates due to malfunction, is very unlikely with current pacemaker technology. In both of these cases, placing a magnet over the pacemaker will switch it from demand to fixed mode and may terminate the tachycardia. Oversensing (C) occurs when the pacemaker senses electrical activity that is not of cardiac origin and erroneously inhibits the generator. This may result in bradycardia. Undersensing (D) occurs when the pacemaker can not adequately sense the intrinsic electrical activity of the heart. If the pacemaker is in an inhibit mode, this can result in the pacemaker firing inappropriately.
References:
1. Sgarbossa EB, Pinski SL, Barbagelata et al. Electrocardiographic diagnosis of evolving acute myocardial infarction in the presence of left bundle-branch block. N Engl J Med. 1996 Feb 22;334(8):481
2. Smith SW, Dodd KW, Henry TD et al. Diagnosis of ST-elevation myocardial infarction in the presence of left bundle branch block with the ST-elevation to S-wave ratio in a modified Sgarbossa rule. Ann Emerg Med. 2012 Dec;60(6):766-76.
3.Cai Q, Mehta N, Sgarbossa EB, Pinski SL, Wagner GS, Califf RM, Barbagelata A. The left bundle-branch block puzzle in the 2013 ST-elevation myocardial infarction guideline: from falsely declaring emergency to denying reperfusion in a high-risk population. Are the Sgarbossa Criteria ready for prime time? Am Heart J. 2013 Sep;166(3):409-13. doi: 10.1016/j.ahj.2013.03.032.