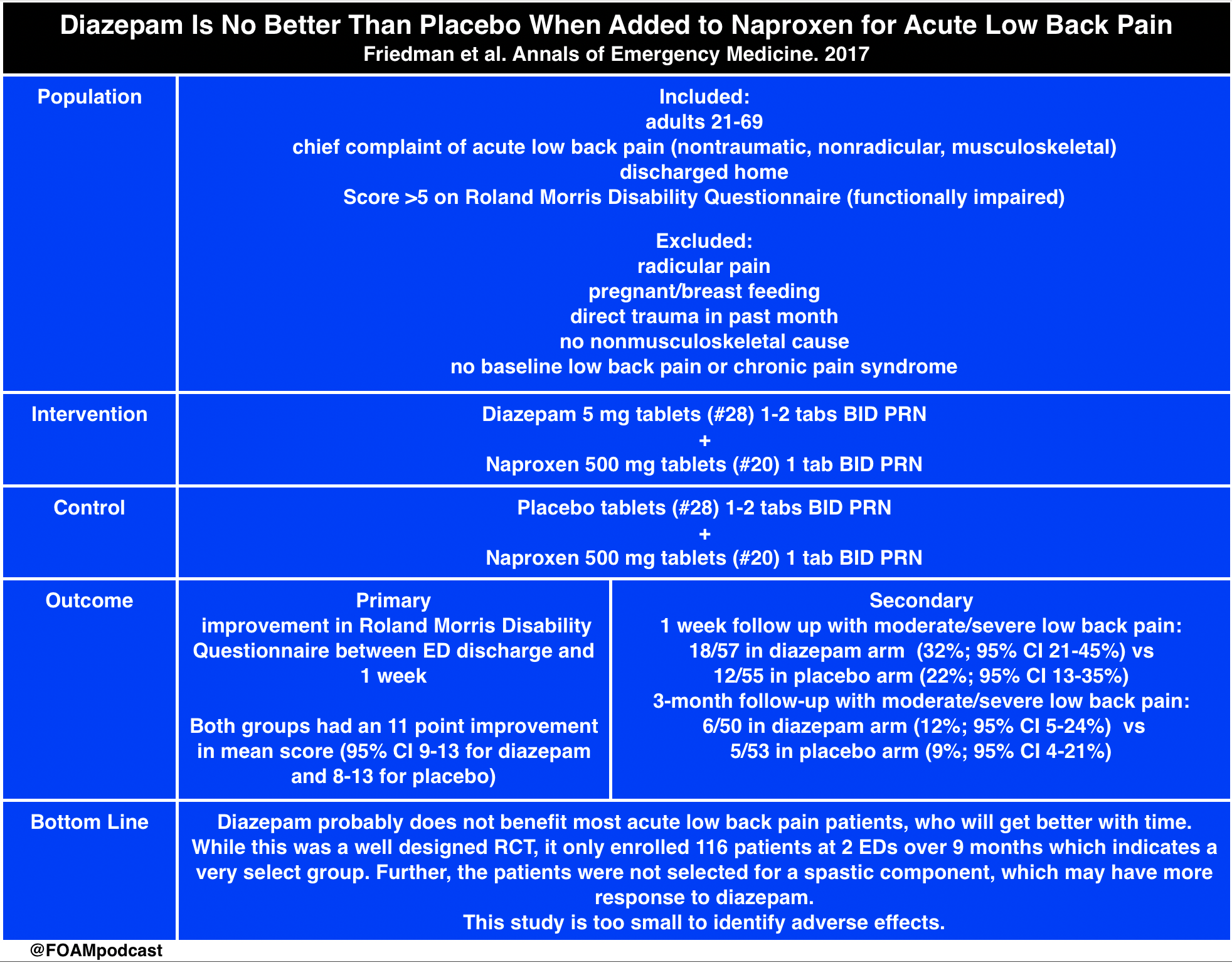
- We cover a post from the fantastic St. Emlyn’s team which breaks down a recently published article in Annals of Emergency Medicine comparing diazepam with placebo in patients with acute low back pain. We recommend you read the full text of the article by Friedman et al.
Core Content
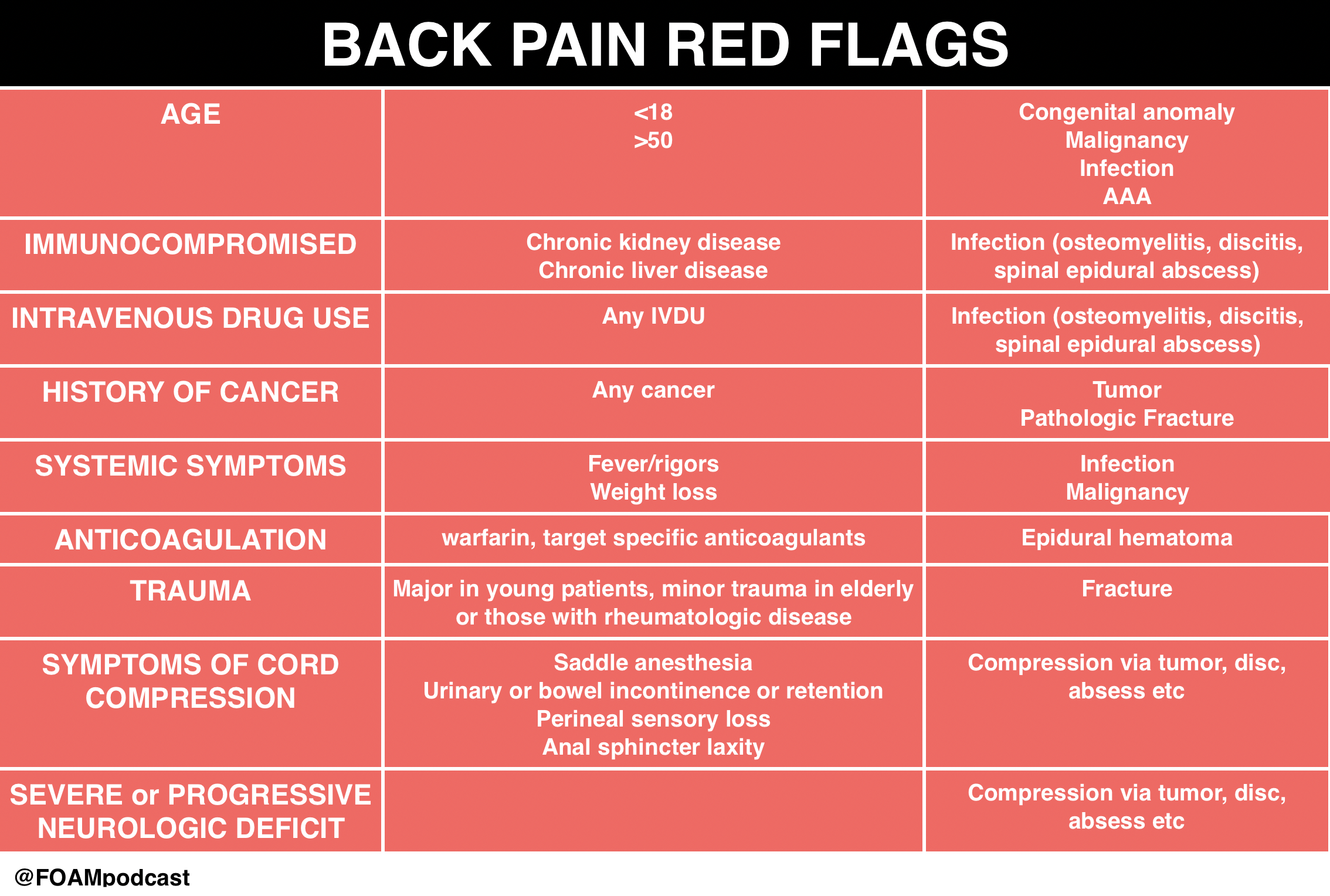
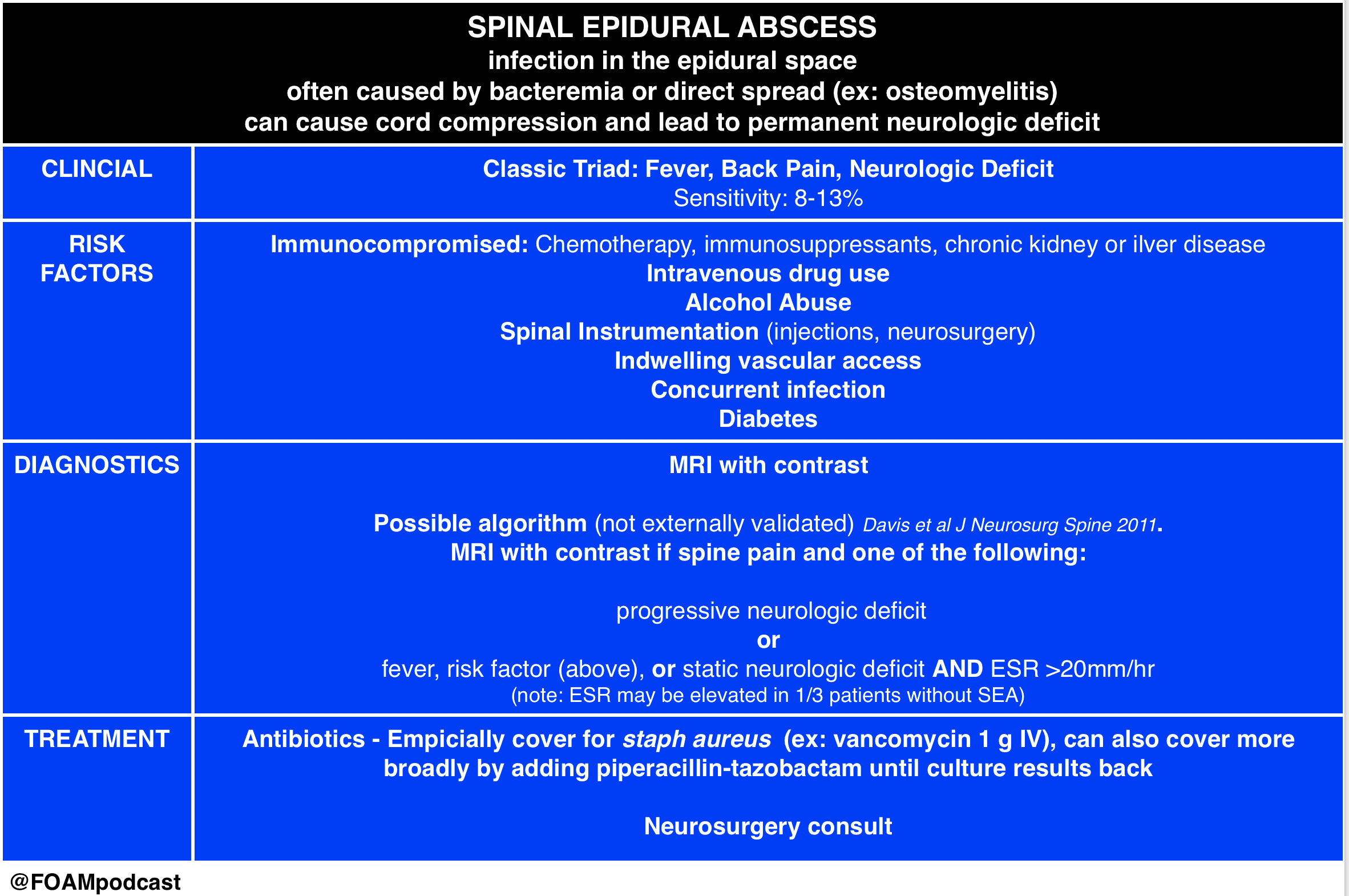
We delve into core content on red flags in back pain and spinal epidural abscess using Rosen’s Emergency Medicine and Tintinalli’s Emergency Medicine Chapter 279 as a guide.
Rosh Review Emergency Board Review Questions
- A 13-year-old boy on chemotherapy for acute lymphoblastic leukemia presents with progressive lower back pain for 2 weeks. Per mom, he has had subjective fevers and a “bulge in his lower back” that is warm to touch. He is currently afebrile and has no focal neurologic deficits. An MRI is obtained as seen in the image above. Which of the following regarding this patient’s condition is true?
A. An appropriate antibiotic regimen is cefepime and metronidazole
B. Direct extension of skin and soft tissue infections is the most common cause
C. Erythrocyte sedimentation rate is a sensitive screening tool
D. Most patients present with back pain, fever, and a focal neurologic deficit
[accordion]
[toggle title=”Answer” state=”closed”]
C. Erythrocyte sedimentation rate is a sensitive screening toolThe patient has a posterior epidural abscess with adjacent osteomyelitis and myositis. The most common cause of an epidural abscess is hematogenous spread of infection, not direct extension from skin or soft tissue infection. Major risk factors include diabetes, intravenous drug abuse, chronic renal failure, alcoholism, and immunosuppression. The most common organism involved is Staphylococcus aureus. Other organisms include streptococci, anaerobes, gram-negative bacilli, and Pseudomonas aeruginosa. Patients present with localized back pain with tenderness to percussion. Fevers are common (reported in up to 75% of patients). MRI is the diagnostic modality of choice, but erythrocyte sedimentation rate is a sensitive marker and may be used in conjunction with plain radiographs to screen for infectious spinal disease.Vancomycin is an important component of the antibiotic regimen because it covers methicillin-resistant Staphylococcus aureus (MRSA) and is usually combined with a 3rd-generation cephalosporin (A). Cefepime is a 4th-generation cephalosporin with pseudomonas coverage. Metronidazole or clindamycin can be added for anaerobic coverage. While the classic triad consists of back pain, fever, and neurologic deficits (D), only a small proportion of patients actually have all three components at presentation. The most common cause of an epidural abscess is hematogenous spread of infection, not direct extension from skin or soft tissue infection (B).
[/toggle]
[/accordion]
An 8-year-old previously healthy boy presents with back pain and fever for 4 days. He complains of pain in the low back, which is increased with bending or twisting. The pain radiates down into his left leg. He denies trauma. Physical exam is remarkable only for tenderness to palpation over the lumbar spine. What management is indicated
A. Ibuprofen and follow up with his pediatrician
B. MRI of the lumbar spine
C. Plain radiographs of the lumbar spine
D. Urinalysis
[accordion]
[toggle title=”Answer” state=”closed”]
B.
MRI of the lumbar spine. This patient presents with symptoms consistent with discitis and should have an MRI for diagnosis. Discitis is a rare infection of the nucleus pulposus and can involve the cartilaginous endplate and vertebral body. It can occur spontaneously or after surgical procedures. Typically, patients present with severe pain localized to the spinal level of involvement. Any movement of the spine exacerbates the pain. Children often present with sudden onset of back pain and refusal to walk. The lumbar spine is most commonly involved and the average age of patients is 7 years. Radicular symptoms are common (present in 50-90% of cases) and most patients will present with fever (90%). Neurologic deficits are uncommon. Serious pathology should be suspected in any pediatric patient presenting with back pain. Neurologic symptoms are rarely present. MRI is the best study for diagnosis and can also rule out other critical diagnoses including epidural abscess. Laboratory studies are non-specific and insensitive but typically will have an elevated erythrocyte sedimentation rate. White blood cell counts are frequently within the normal range.
[/toggle]
[/accordion]