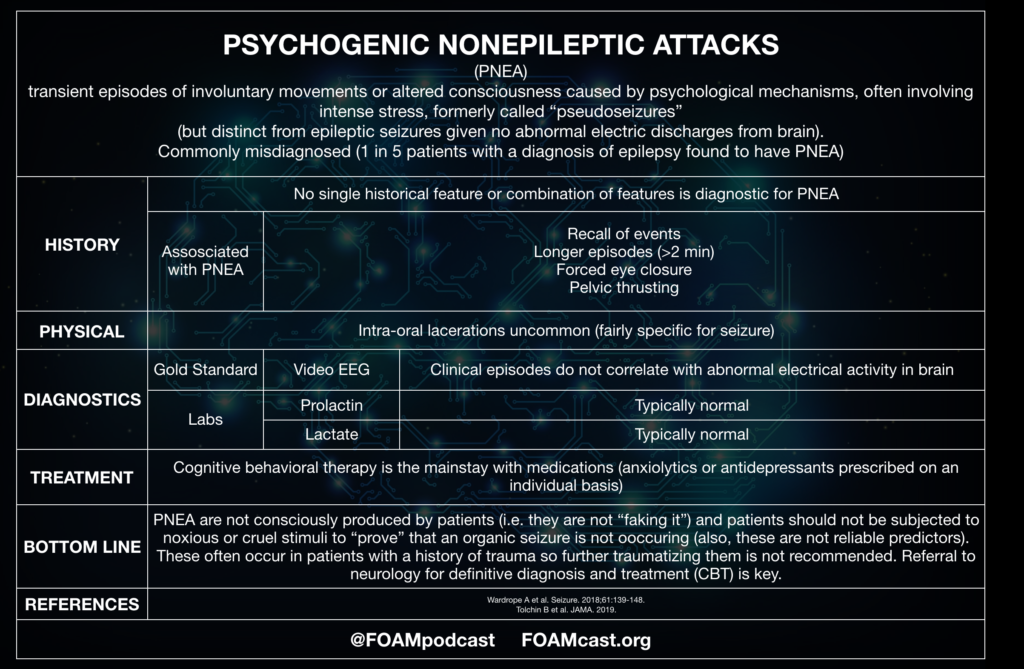
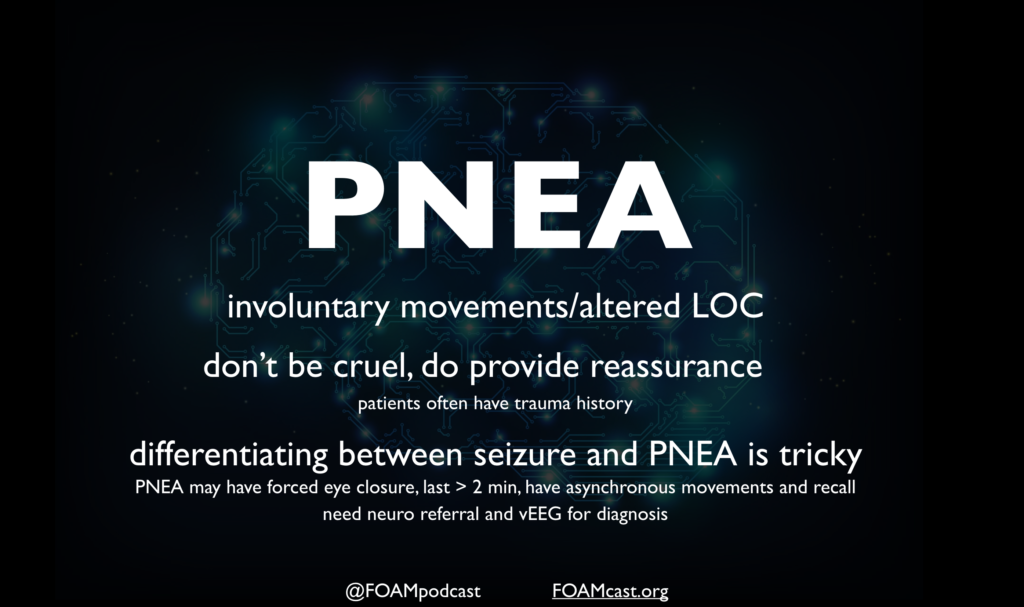
Psychogenic non-epileptic attacks (PNEA) have been formally referred to as pseudoseizures or psychogenic non-epileptic seizures. Recently, this entity has been rebranded to PNEA to reflect that there is no actual seizure activity and potentially prevent confusion and mislabeling among patients.
A 10-year-old girl presents with episodes of brief staring spells that she is unaware of. The patient’s mother states that the onset and termination of the spells are abrupt. The patient is otherwise healthy. She has lots of friends at school and has excellent academic performance. Physical examination and laboratory studies are normal at this time. Which of the following is the most likely diagnosis?
- Absence seizure
- Attention deficit hyperactivity disorder
- Autism spectrum disorder
- Complex partial seizure
[accordion]
[toggle title=”Answer” state=”closed”]
- Absence seizure is a type of generalized seizure characterized by loss of consciousness sometimes accompanied by myotonic, atonic, clonic, or tonic components, autonomic components (e.g., enuresis), or automatisms. The onset of absence seizure commonly occurs in early childhood with a predilection to the female sex. It usually terminates by the age of 20 years or may transform into another form of generalized seizure. Absence seizure may be typical or atypical. The onset and termination of a typical absence seizure are abrupt while they may be gradual in an atypical absence seizure. Additionally, atypical seizure commonly occurs in patients with multiple seizure types and demonstrates more marked changes in tone. Patients with an atypical absence seizure may also have a developmental delay or mental retardation. Patients with absence seizure may miss a few words or break off mid-sentence during an attack. The attack period is so brief that the patient is unaware of it. Physical examination may be normal. Having the child hyperventilate for three to five minutes may precipitate a staring attack. Diagnosis of typical absence seizure is with electroencephalography that shows bursts of bilateral synchronous and symmetric 3-Hertz spike-wave activity. A slower spike-wave discharge is noted in an atypical absence seizure. Treatment is with antiepileptic medications including ethosuximide and valproic acid. All patients with absence seizure should be referred to a neurologist for management. Drug levels of valproic acid should be monitored.While attention deficit hyperactivity disorder (B) has a childhood onset, it is marked by symptoms of inattentiveness, hyperactivity, and impulsivity that are not present in the vignette above. Autism spectrum disorder (C) may also have an early onset. However, patients suffer from pervasive difficulties with social communication and repetitive interests and behavior that are absent in the vignette above. In complex partial seizure (D), the duration of seizure usually lasts > 30 seconds, automatisms are present, and the termination of the seizure is gradual.
[/toggle]
[/accordion]
References:
- Lafrance WC, Baker GA, Duncan R, Goldstein LH, Reuber M. Minimum requirements for the diagnosis of psychogenic nonepileptic seizures: a staged approach: a report from the International League Against Epilepsy Nonepileptic Seizures Task Force. Epilepsia. 2013;54(11):2005-18.
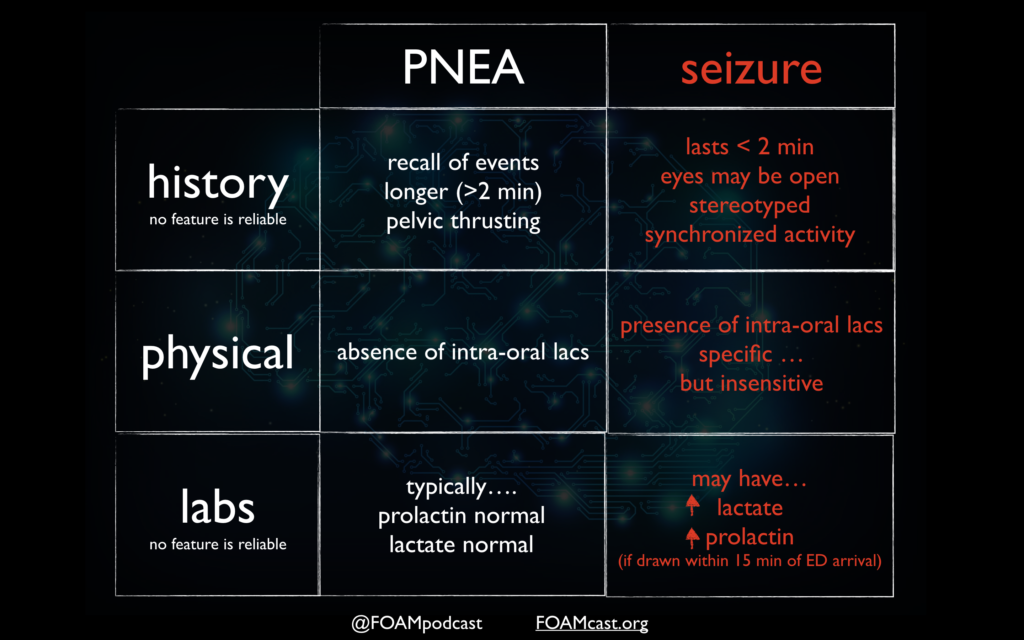
- Wardrope A, Newberry E, Reuber M. Diagnostic criteria to aid the differential diagnosis of patients presenting with transient loss of consciousness: A systematic review. Seizure. 2018;61:139-148.
- Chen et al. Value of witness observations in the differential diagnosis of transient loss of consciousness. Neurology. 2019 Feb 26;92(9):e895-e904. doi: 10.1212/WNL.0000000000007017. Epub 2019 Jan 25.
- Shmuely S, Bauer PR, Van zwet EW, Van dijk JG, Thijs RD. Differentiating motor phenomena in tilt-induced syncope and convulsive seizures. Neurology. 2018;90(15):e1339-e1346.
- Doğan EA, Ünal A, Ünal A, Erdoğan Ç. Clinical utility of serum lactate levels for differential diagnosis of generalized tonic-clonic seizures from psychogenic nonepileptic seizures and syncope. Epilepsy Behav. 2017;75:13-17.