Thromboelastography (TEG) or its related counterpart rotational thromboelastometry (ROTEM) have gained in popularity over the past several years. These tests assess viscoelastic clot strength in whole blood. These tests may offer more granular and potentially reliable information on the patient’s clot formation and fibrinolytic state than traditional measures of coagulation such as International Normalized Ratio (INR), partial thromobplastin time (PTT), and prothrombin time (PT).
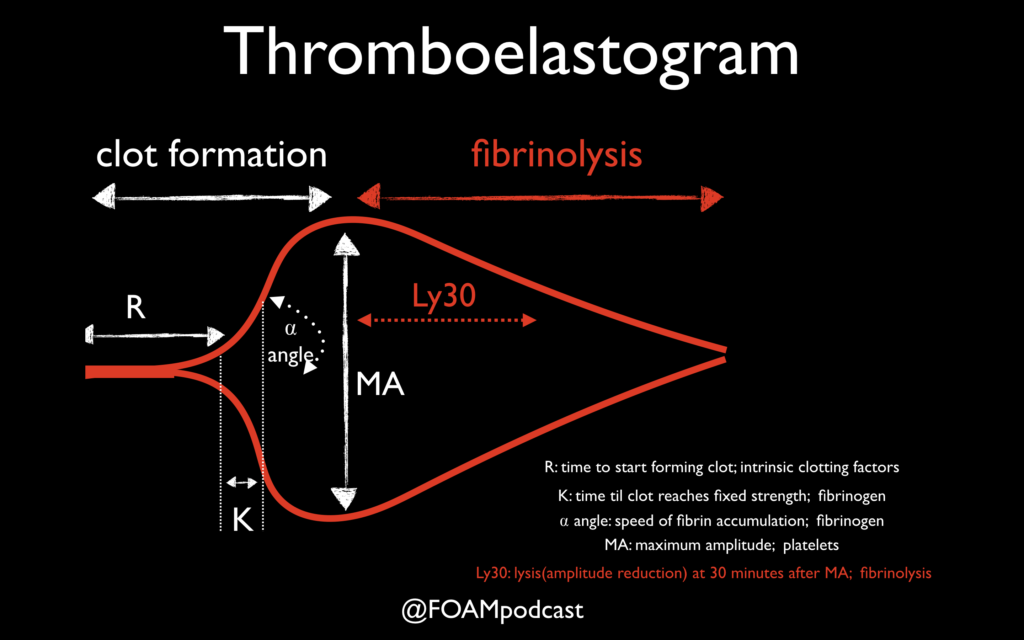
One of the primary advantages to TEG/ROTEM is the ability to target transfusion related therapies to the patient’s overall coagulation profile. Below are some common patterns that emerge and the recommended therapies.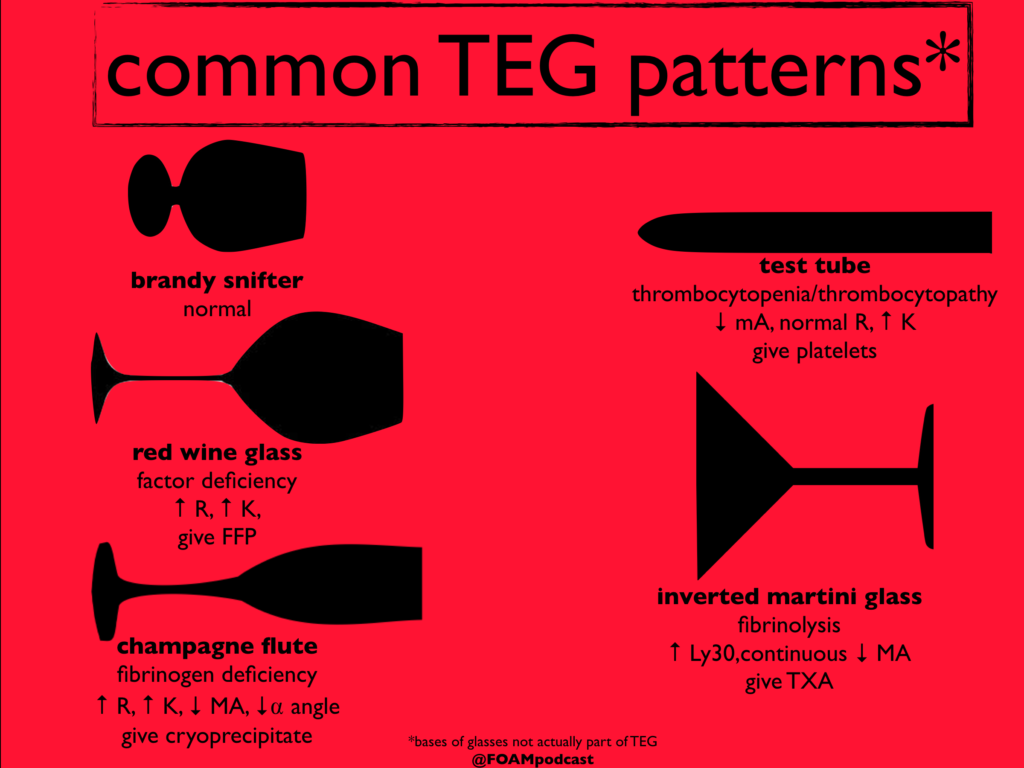
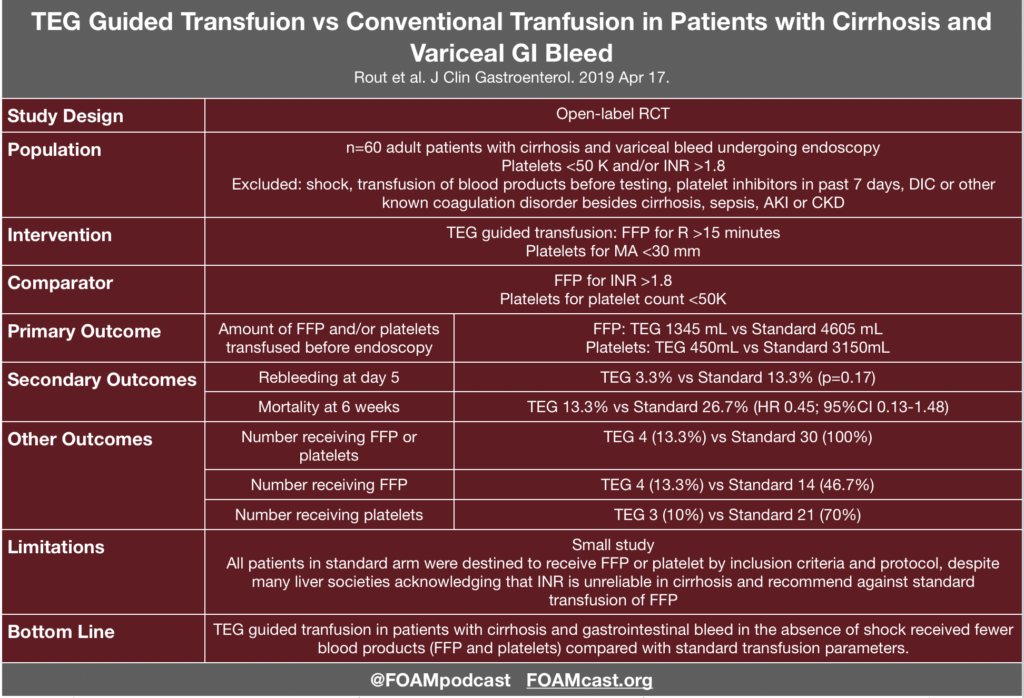
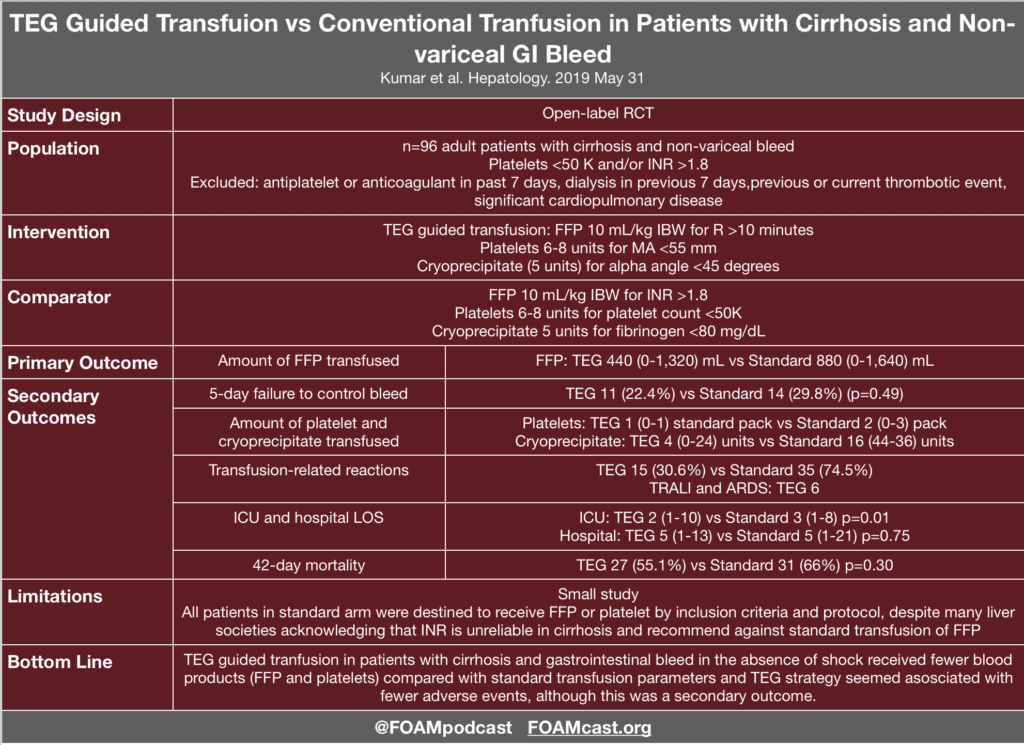
Evidence for TEG in Cirrhosis
Additional FOAM resources: PulmCrit
References:
- Wikkelsø A, Wetterslev J, Møller AM, Afshari A. Thromboelastography (TEG) or thromboelastometry (ROTEM) to monitor haemostatic treatment versus usual care in adults or children with bleeding. Cochrane Database Syst Rev. 2016;(8):CD007871.
- Kumar M, Ahmad J, Maiwall R, et al. Thromboelastography-Guided Blood Component Use in Patients With Cirrhosis With Nonvariceal Bleeding: A Randomized Controlled Trial. Hepatology. 2019; In Press
- Rout G, Shalimar, Gunjan D, et al. Thromboelastography-guided Blood Product Transfusion in Cirrhosis Patients With Variceal Bleeding: A Randomized Controlled Trial. J Clin Gastroenterol. 2019; In Press.
- Goodman MD, Makley AT, Hanseman DJ, Pritts TA, Robinson BR. All the bang without the bucks: Defining essential point-of-care testing for traumatic coagulopathy. J Trauma Acute Care Surg. 2015;79(1):117-24.
You are called to the bedside for a postoperative patient who is hypotensive, febrile, and has acute onset of respiratory distress following the initiation of a blood transfusion. Which of the following is the most appropriate initial action in the management of this patient?
A. Apply oxygen
B. Call the blood bank
C. Order steroids
D. Stop the transfusion
[accordion]
[toggle title=”Answer” state=”closed”]
Transfusion-related acute lung injury is a blood transfusion complication characterized by a rapid onset of non-cardiogenic pulmonary edema. The pathogenesis is thought to be a two-part mechanism involving neutrophil sequestration with priming in the lung microvasculature followed by neutrophil activation by a factor in the blood product. Pre-transfusion risk factors include current smoking, chronic alcohol use, liver transplantation surgery, positive fluid balance, shock, and higher ventilated peak airway pressures. Though there is an association of transfusion-related acute lung injury with all blood products, high-plasma-volume products (plasma, apheresis platelet concentrations, and whole blood) have the greatest risk. Clinical presentation may occur immediately after the initiation of the blood transfusion although it can be delayed up to six hours. The patient may rapidly develop acute respiratory distress syndrome, with symptoms that may include hypoxemia, fever, hypotension, cyanosis, pulmonary infiltrates on chest imaging, and if intubated, pink frothy secretions when suctioned. Treatment involves immediate discontinuation of the transfusion followed by supportive care of the acute respiratory distress syndrome. This includes oxygen supplementation and hemodynamic support. Apply oxygen (A), call the blood bank (B), and order steroids (C) are treatments for transfusion-related acute lung injury but are not the most appropriate in the initial management. Discontinuing the transfusion, which is the cause of the acute lung injury, is the immediate need upon identifying the condition.
[/toggle]
[/accordion]