We bring you pearl from the American College of Emergency Physicians (ACEP) 2017 Scientific Assembly.
Pediatric Pitfalls – Dr. Tim Horeczko
Critical Care Literature Updates – Dr. Michael Winters
We bring you pearl from the American College of Emergency Physicians (ACEP) 2017 Scientific Assembly.
Pediatric Pitfalls – Dr. Tim Horeczko
Critical Care Literature Updates – Dr. Michael Winters
In this episode, we summarize recent literature we feel is high yield, important, or frequently discussed in emergency medicine. As always, we encourage you to read the papers and not FOAM it alone.
Antibiotics and abscesses – Daum et al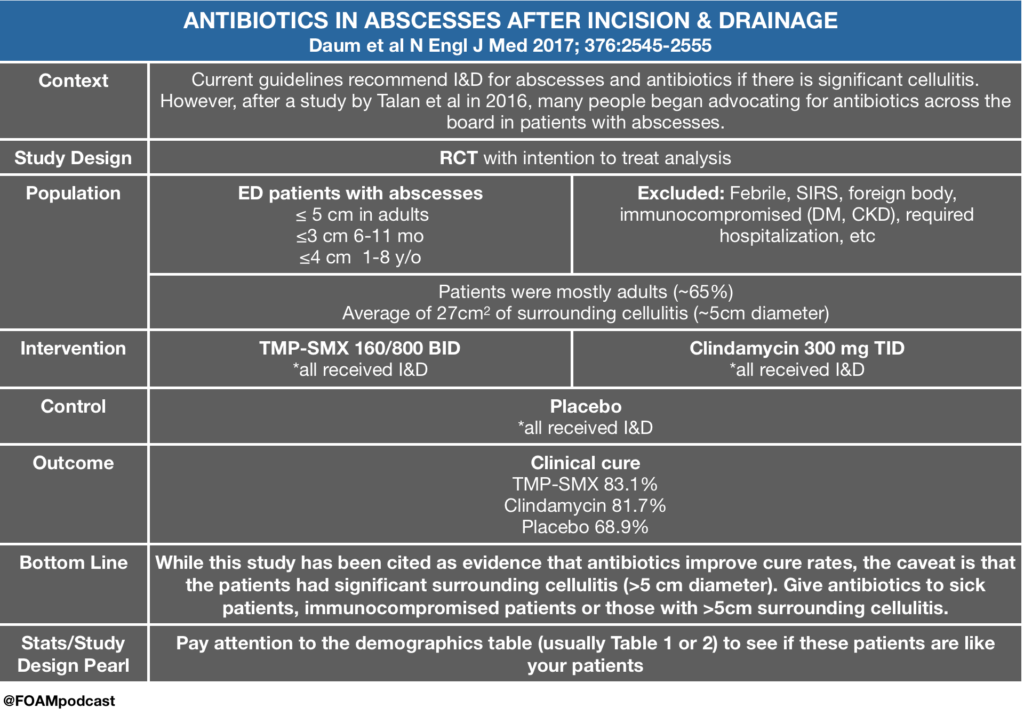
FAST in hemodynamically stable patients – Holmes et al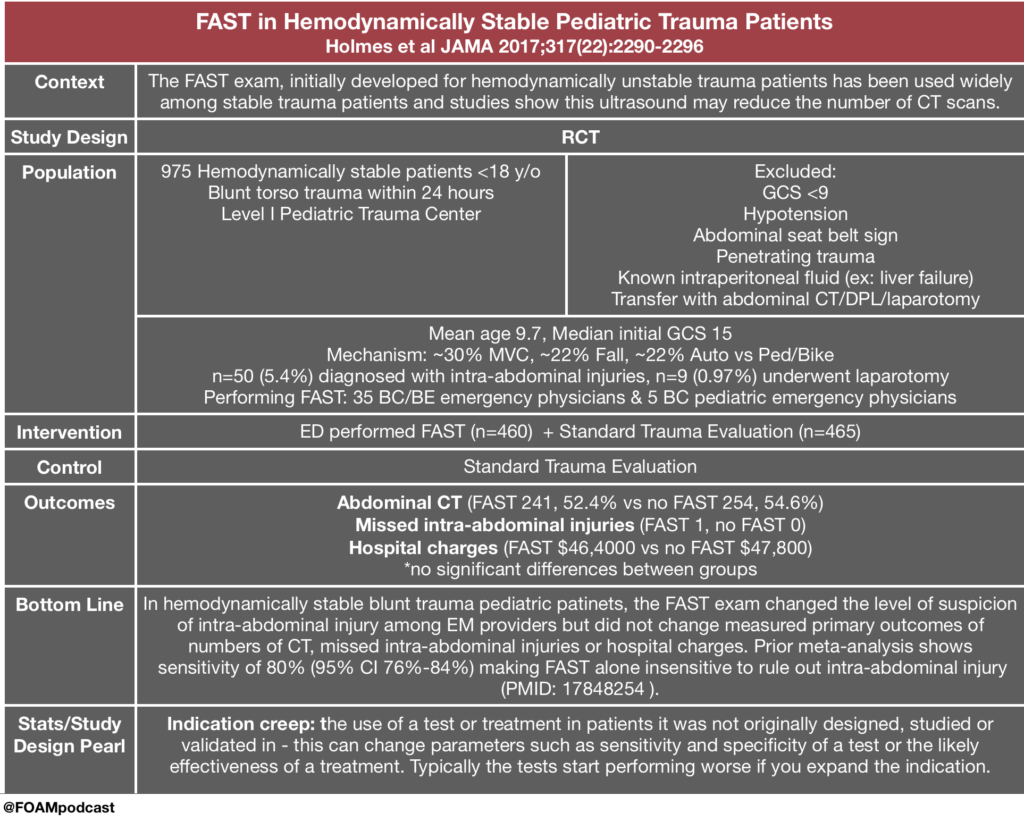
Haloperidol in gastroparesis – Roldan et al and Ramirez et al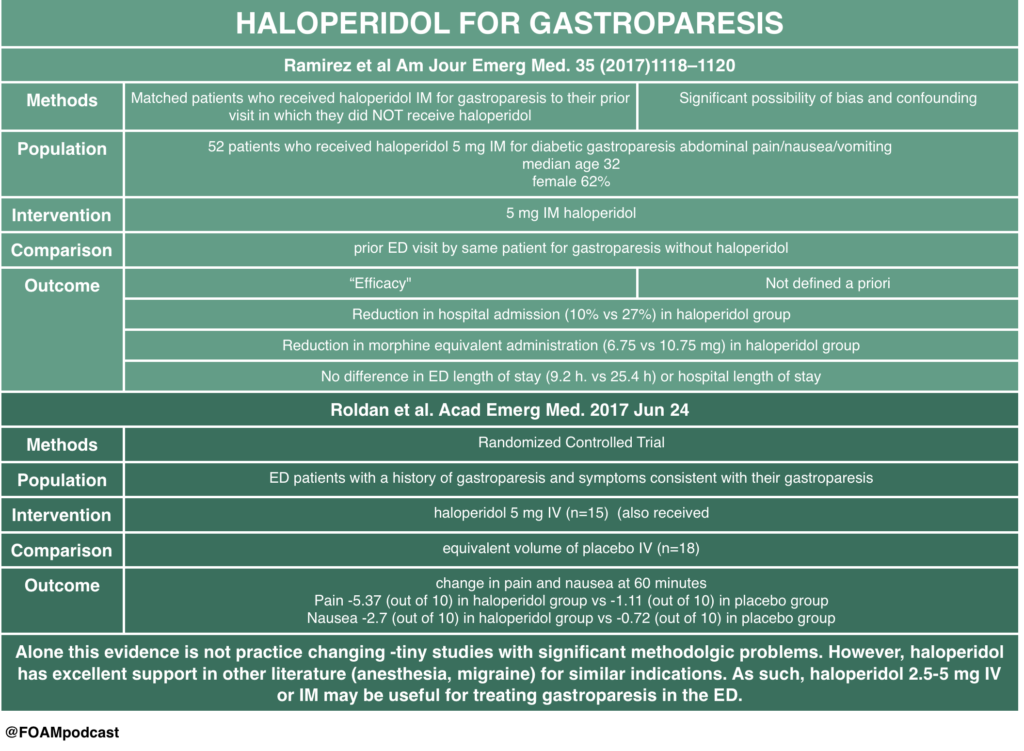
Ignoring PERC – Buchanan et al
Steroids in non-asthma/COPD lower respiratory tract infections – Hay et al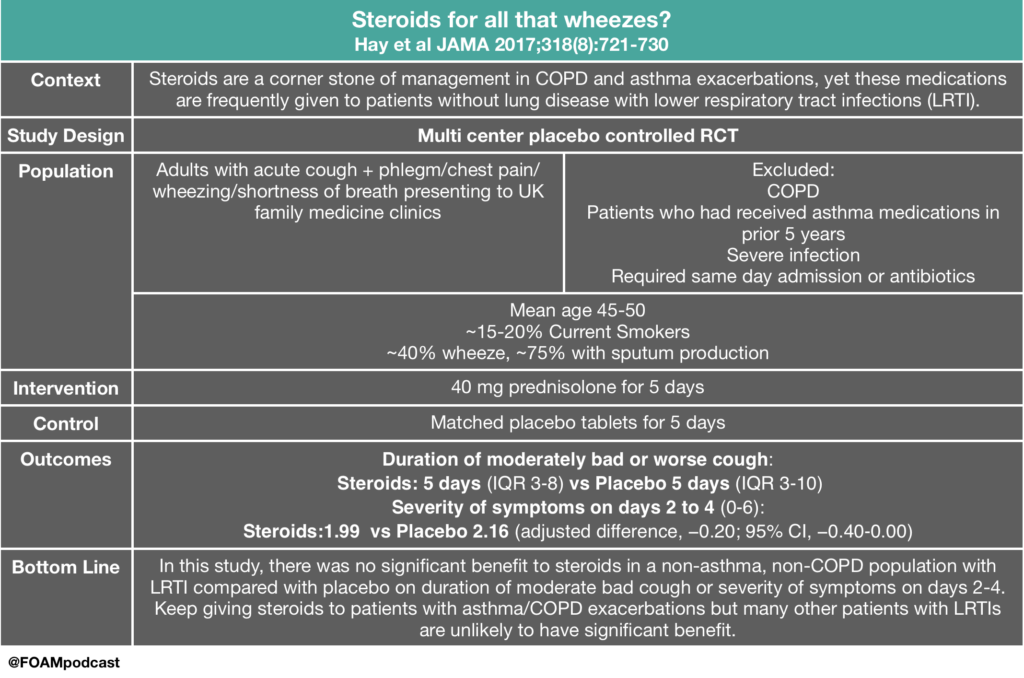 ENDAO – Caputo et al
ENDAO – Caputo et al
Gender pay gap persists in academic EM (and it’s not due to hours, rank, or roles) – Madsen et al
We review this blog post by Bryan Hayes, an ED pharmacist (@PharmERToxGuy), on the use of physostigmine in anticholinergic toxicity.
We review core content on anticholinergic toxicity using Rosen’s Emergency Medicine (9th ed), Tintinalli’s Emergency Medicine (8th ed) and Goldrank’s Toxicology as guides.
Rosh Review Emergency Board Review Questions
A 27-year-old man is brought to the ED by EMS after being found wandering in the street. His BP is 155/70, HR 115, T 37.5°C, RR 16, pulse ox 99% on room air, and finger stick glucose 98. On exam, the patient is confused with mumbling speech. His pupils are 7 mm and nonreactive. His face is flushed. Mucous membranes and skin are dry. Which of the following toxidromes is this patient exhibiting?
A. Anticholinergic
B. Cholinergic
C. Sedative-hypnotic
D. Sympathomimetic
[accordion]
[toggle title=”Answer” state=”closed”]
A. Anticholinergic Toxidrome refers to a constellation of physical findings that can provide important clues in a toxic ingestion. This patient exhibits an anticholinergic toxidrome. Anticholinergics are widely available as over-the-counter cold preparations and sleep aids (diphenhydramine, chlorpheniramine, doxylamine). They also are the basis of the toxicity of jimsonweed. Anticholinergics competitively inhibit acetylcholine in the central and peripheral nervous systems. This classic toxidrome is often described by the phrase “mad as a hatter (altered mental status), blind as a bat (mydriasis), red as a beet (flushed skin), hot as a hare (dry skin due to inability to sweat), dry as a bone (dry mucous membranes).” Other findings include tachycardia, delirium, seizures, and hallucinations. Treatment is mainly supportive with benzodiazepines for agitation and seizures, and cooling for temperature reduction. Gastric decontamination (whole-bowel irrigation or gastric lavage) is often recommended due to the delay in gastric emptying caused by anticholinergics. The use of physostigmine, a reversible cholinesterase inhibitor that will increase synaptic acetylcholine, is controversial and should be administered only in consultation with a toxicologist.
The cholinergic toxidrome (B) is characterized by the mnemonics SLUDGE (salivation, lacrimation, urination, defecation, GI upset, emesis) or DUMBBELS (defecation, urination, miosis, bronchospasm, bronchorrhea, emesis, lacrimation, salivation) and occurs after exposure to organophosphates or carbamates. The sedative-hypnotic toxidrome (C) is seen with benzodiazepines and barbiturates. Clinically, patients exhibit central nervous system and respiratory depression. The sympathomimetic toxidromes (D) can occur after ingestion of cocaine, amphetamines, or decongestants. It typically presents with delirium, paranoia, tachycardia, hypertension, hyperpyrexia, diaphoresis, mydriasis, seizures, and hyperactive bowel sounds. Sympathomimetic and anticholinergic toxidromes are frequently difficult to distinguish. The key difference is that sympathomimetics are associated with diaphoresis, whereas anticholinergics cause dry skin.
[/toggle]
[/accordion]
A 22-year-old man is brought into the Emergency Department by Emergency Medical Services with altered mental status. He is an agitated man and mumbling incoherent words. His pupils are 6 mm and reactive to light. His axillae are dry. His heart rate is 115 beats/minute and temperature is 101.6 oF. Which of the following is a complication of the antidote used in the treatment of this condition?
A. Asystole
B. Bladder retention
C. QT-interval prolongation
D. Respiratory depression
[accordion]
[toggle title=”Answer” state=”closed”]
Asystole. The mnemonic for the anticholinergic toxidrome is blind as a bat (mydriasis), red as a beet (vasodilation leading to flushing), hot as a hare (hyperthermia), dry as a bone (dry skin and mucosa), mad as a hatter (visual or auditory hallucinations, agitation, and mumbling or incoherent speech), bloated as a toad (ileus and urinary retention), and the heart runs alone (tachycardia). Additionally, anticholinergic toxicity can cause orthostatic hypotension (especially in the elderly), picking behavior, and can lead to seizures, coma, and even death. There are multiple anticholinergic medications, including tricyclic antidepressants, antihistamines, antiparkinson medications, antipsychotics, antispasmodics, belladonna alkaloids, skeletal muscle relaxants, and mydriatics. Antihistamine overdose is the most common cause of anticholinergic toxicity. Treatment is supportive with IV hydration. If the ingestion occurred within one hour, GI decontamination with activated charcoal is reasonable. Benzodiazepines are used for significant agitation and seizures. Good temperature control should be achieved with antipyretics and active cooling is essential. For wide complex tachyarrhythmias, treatment is with sodium bicarbonate. The antidote is physostigmine, a reversible acetylcholinesterase inhibitor. There is, however, a risk of profound bradycardia, seizures, and asystole in patients with widened QRS complexes. This risk is minimal if there is a pure anticholinergic syndrome without concomitant sodium channel blockade, but this is unfortunately not always known. Since the most common cause of anticholinergic toxicity is from diphenhydramine overdose (which causes sodium channel blockade), physostigmine should only be used with the assistance of a medical toxicologist.
[/toggle]
[/accordion]
References:
Dr. Salim Rezzaie of RebelEM wrote a blog post on HUGS – Haloperidol for Gastroparesis. This study had significant methodologic limitations but provides some interesting insight into a practice that many providers have adopted – using haloperidol for gastroparesis. A tiny RCT by Roldan and colleagues also looked at this practice and found promising results, although the study was very small. Haloperidol has also been used in cannabinoid hyperemesis but literature on this is limited to case reports/series.
Core Content
We review biliary colic, cholecystitis, and cholangitis using Tintinalli (8th ed) Chapter 79 and Rosen’s Emergency Medicine (9th ed) Chapter 80 as guides.
Rosh Review Emergency Board Review Questions
A 60-year-old woman presents with two days of right upper quadrant abdominal pain constant in nature and associated with subjective fever, nausea, and vomiting. Vital signs are temperature of 38.1°C, heart rate 87, blood pressure 140/80 mm Hg, respiratory rate 14, and oxygen saturation of 99% on room air. Her abdomen is soft with right upper quadrant tenderness and a positive Murphy’s sign. Which of the following tests is most sensitive and specific in diagnosing this patient’s condition?
A. Computed tomography scan with intravenous contrast
B. Hepatobiliary iminodiacetic acid (HIDA) scan
C. MRI with gadolinium
D. Ultrasound
[accordion]
[toggle title=”Answer” state=”closed”]
This patient has suspected acute cholecystitis and requires an imaging study for confirmation. Hepatobiliary iminodiacetic acid (HIDA) scanning is considered the most sensitive and specific test for diagnosing acute cholecystitis. IDA is administered intravenously, taken up by hepatocytes, and excreted into the bile canaliculi. Failure to obtain an outline of the gallbladder within one hour proves cystic duct obstruction and, in the appropriate clinical setting, confirms the diagnosis of acute cholecystitis. Visualization of the gallbladder and common duct within one hour has a high negative predictive value. A HIDA scan is usually obtained when the ultrasound study is equivocal.
Computed tomography scan with intravenous contrast (A) can identify cholecystitis with a reported sensitivity of 92% and specificity of 99%. It is most useful in cases of emphysematous and hemorrhagic cholecystitis. MRI with gadolinium (C) provides similar diagnostic yield to CT scan. Ultrasound (D) is most useful in the ED setting because it is a quick, noninvasive test. Its sensitivity and specificity, however, are lower than a HIDA scan’s for pathology-confirmed cholecystitis. Ultrasound findings and a clinical exam consistent with acute cholecystitis are highly predictive, and many such patients will undergo cholecystectomy without further diagnostic testing.
[/toggle]
[/accordion]
References:
Did you think blood pressure cuff readings were accurate? Guess again.https://t.co/vQc6BV2UGD @JACCJournals pic.twitter.com/f36ppi3Hrl
— Eric Topol (@EricTopol) July 25, 2017
Picone et al published a meta-analysis in the Journal of the American College of Cardiology discussing the accuracy of cuff blood pressures.
We cover core content on hypertension using the ACEP clinical policy on hypertension, Rosen’s (9th ed) Chapter 74 “Hypertension,” and Tintinalli (8th ed), Chapter 57 “Systemic Hypertension” Chapter 59 “Aortic Dissection and Related Aortic Syndromes” as guides. Check out this FOAM review of hypertension in the ED.
References:
We cover Free Open Access Medical Education on opioids.
The Poison Review podcast reviews papers on the opioid epidemic, including a paper by Rudd et al demonstrating an increase in opioid-related deaths over the past five years as well as the following paper by Shah and colleagues.
The Dantastic Mr. Tox and Howard, a new podcast on the scene, also covers multiple topics on opioids, including common misconceptions of tramadol.
The American College of Medical Toxicology recently released a statement on fentanyl exposure, stating how absolutely unlikely it is that accidental dermal exposure would result in toxicity. ” If bilateral palmar surfaces were covered with fentanyl patches, it would take approximately 14 minutes to receive 100 mcg of fentanyl…This extreme example illustrates that even a high dose of fentanyl prepared for transdermal administration cannot rapidly deliver a high dose.”
We cover core content on opioid overdose and withdrawal using Rosen’s Emergency Medicine (9th ed) Chapter 156 and Tintinalli’s Emergency Medicine (8th ed), Chapter 186 as a guide.
We are in Berlin for #dasSMACC and have lots of pearls to share from the speakers at this amazing conference. Talks will be released for free on the SMACC podcast over the next year, but this podcast holds some pearls that we thought couldn’t wait.
Overall trope of the conference….
for more on the Dunning-Kruger effect check out this post
Drs. Jacob Avila and Ben Smith on Airway Ultrasound
Check out this 7-minute video on ETT placement confirmation using ultrasound
Dr. James Rippey on Point of Care Ultrasound Incidental Findings
Dr. Jack Iwashyna on Persistent Critical Care
We are in Berlin for #dasSMACC and have lots of pearls to share from the speakers at this amazing conference. Talks will be released for free on the SMACC podcast over the next year, but this podcast holds some pearls that we thought couldn’t wait.
Dr. Leanne Harnett on Pulmonary Embolism with Right Heart Thrombus (PE with RHT)
Drs. Reuben Strayer (@emupdates) and Scott Weingart (@emcrit) on Acute Hypertensive Pulmonary Edema
Dr. Michele Domico on Pediatric Cardiology Emergencies
Dr. Haney Mallemat (@CriticalCareNow) on Transesophageal Echocardiography (TEE) during Cardiac Arrest
For more on pulse checks, see this blog post.
References:
We are at #dasSMACC in Berlin thanks to the Rosh Review. All talks will be released for free on the SMACC podcast over the next year, but meanwhile, we wanted to share some pearls from the conference.
Dr. Brian Burns (@HawkmoonEMS) on trauma
Dr. David Carr (@davidcarr333)
Dr. Paul Young (@DogICUma)
Dr Jess Mason (@JessMasonMD)
We interrupt our normal core content to cover an important topic highlighted in JAMA’s recent article, “Medical Texting and Protected Health Information. What is permitted?“
Other pearls:
Reference:
Department of Health and Human Services. “Guidance Regarding Methods for De-identification of Protected Health Information in Accordance with the Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule.” November 16, 2015