We are in Las Vegas at ACEP 2016 and discuss high yield or cutting edge lectures each day.
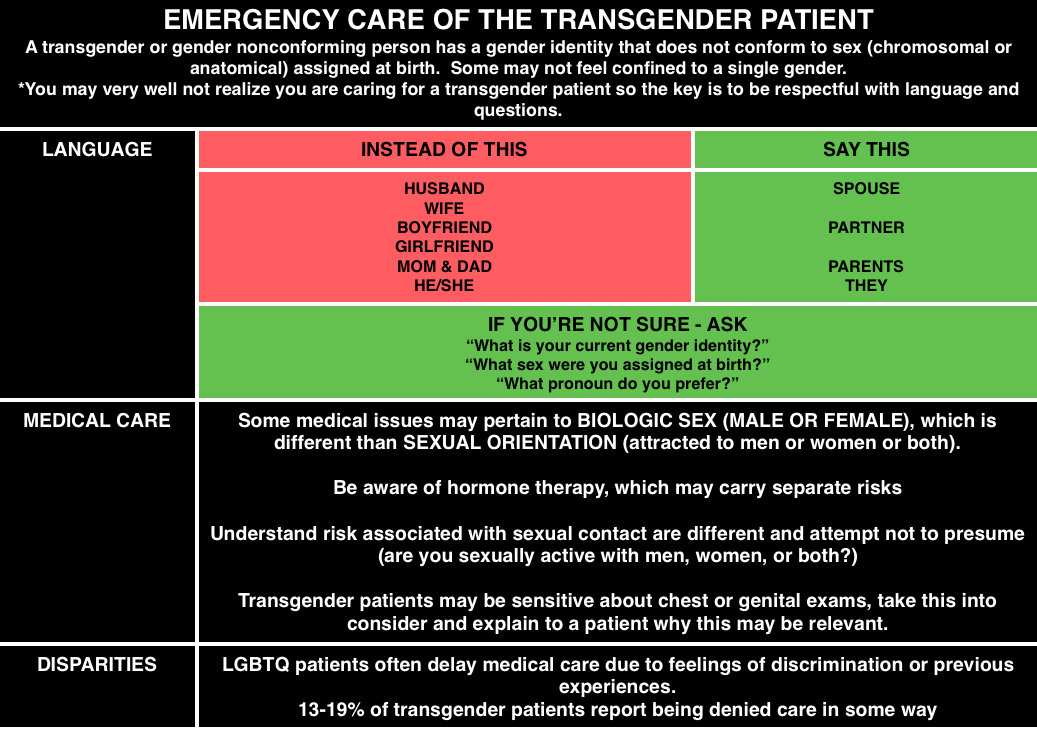
Dr. Anne Daul – Emergency Care of the Transgender Patient
Most emergency medicine physicians and trainees lack training in caring for LGBTQ patients, let alone transgender patients [1]. Many members of the LGBTQ community may have delays in medical care including 21% of transgender patients in a Canadian survey[2]. Also, according to a 2010 task force, 19% of transgender patients report being denied care in some way [3].
Here is a video from SMACC Dublin from Thom O’Neill on caring for LGBT youth
https://www.youtube.com/watch?v=7ZsYgftEv2U&feature=youtu.be
Check out these FOAM resources from EPMonthly and Mayo.
Dr. David Callaway – Active Shooter
2% of active shooter events take place in the health care setting.
Plan of Action in Active Shooter Scenario: AVOID DENY DEFEND TREAT
- Avoid – stay away from the shooter.
- Deny – deny them access to you or the area. Lock doors, block pathways, turn off the lights, make it more difficult for them.
- Defend -.if necessary, defend yourself.
- Treat – once you are safe, and the scene is safe, treat and care for your patients.
Dr. Kevin Klaur – Lawsuits
Documentation and discharge instructions repeatedly come up in lawsuits.
- Documentation: If you document after the fact, particularly if there was a bad outcome – be straightforward that you are documenting after the fact. Do not document as though you do now know the outcome
- Discharge – lawsuits often come up because discharge instructions or documentation were not sufficient. Klauer argues that it is not sufficient to state “patient improved, discharged home.” He urges us to document a repeat exam or show HOW they are improved.
Dr. Klauer also gave some general pearls on lawsuits – high numbers for orthopedics/missed fractures and administration of RhoGham. An additional pearl he gave was for cauda equina.
- These patients often have small post void residuals because it’s a neurogenic problem, not a mechanical obstruction. Thus, if a patient has other features and has a post void residual of 100 cc, it’s not necessarily not cauda equina.
One ACEP16 lecturer talked about magnesium use in alcohol withdrawal – probably not ready for prime time, Cochrane agrees [4].
References:
- Moll J, Krieger P, Moreno-Walton L. The prevalence of lesbian, gay, bisexual, and transgender health education and training in emergency medicine residency programs: what do we know? Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 21(5):608-11. 2014. [pubmed]
- Bauer GR, Scheim AI, Deutsch MB, Massarella C. Reported emergency department avoidance, use, and experiences of transgender persons in Ontario, Canada: results from a respondent-driven sampling survey. Annals of emergency medicine. 63(6):713-20.e1. 2014. [pubmed]
- Grant JM, Mottet LA, Tanis JD et al. National Transgender Discrimination Survey Report on health and health care Findings of a Study by the National Center for Transgender Equality and the National Gay and Lesbian Task Force. October 2010
- Tejani SM. Magnesium for the prevention or treatment of alcohol withdrawal syndrome in adults. June 2013
One thought on “Care of transgender patients + more from ACEP”
Comments are closed.