The Free Open Access Medical Education (FOAM)
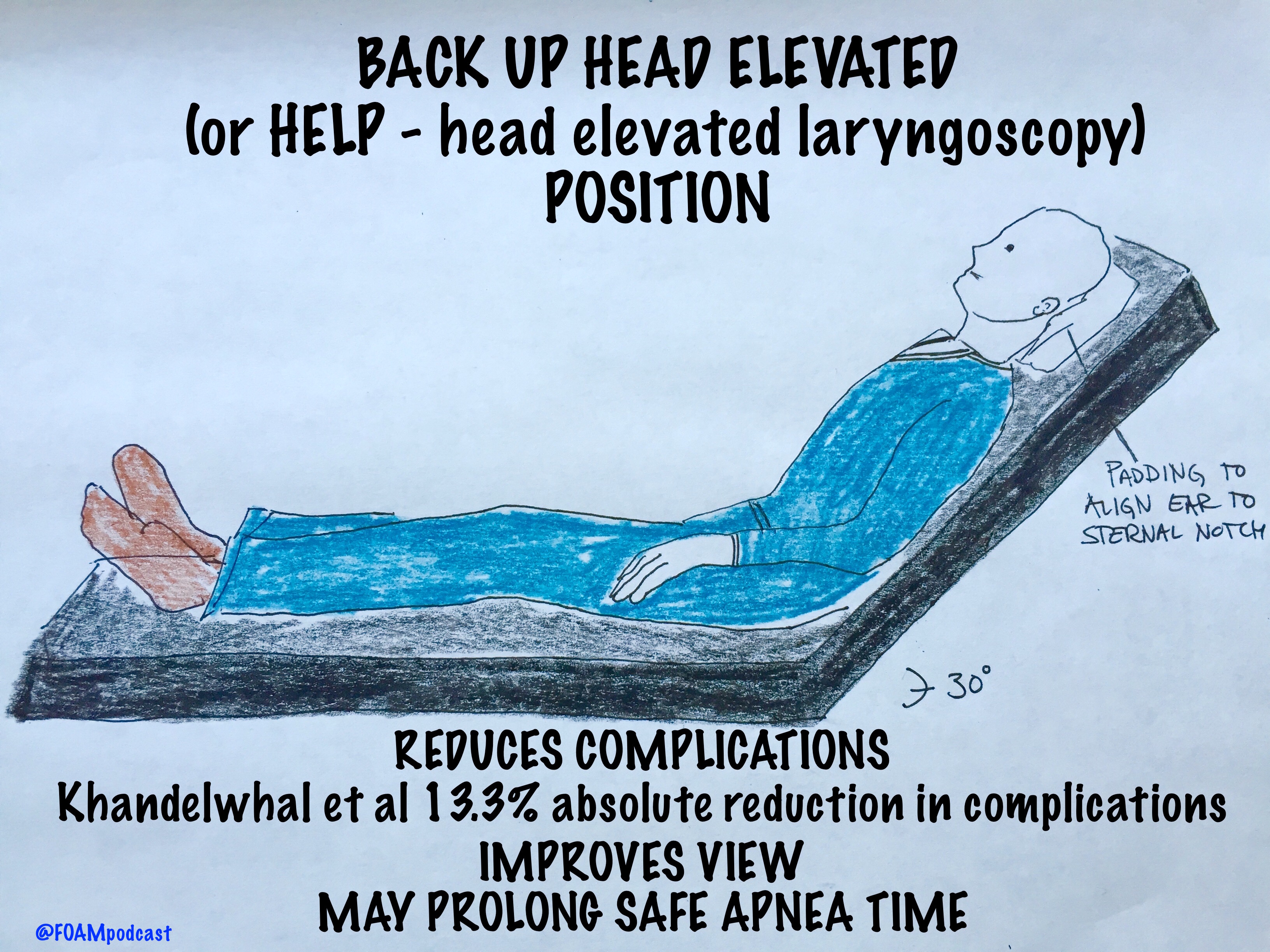
We cover a Scancrit post on the Back Up Head Elevated (BUHE) intubation position. This post details a multicenter retrospective observational study by Khandelwal et al in Anesthesia & Analgesia
Population: 528 adults undergoing emergent intubation
Intervention: Head up at least 30 degrees during intubation
Control: Supine intubation
Primary Outcome: Occurrence of intubation related complication (difficult intubation: >3 attempts or prolonged intubation, hypoxemia, esophageal intubation, or pulmonary aspiration) – 22.6% in supine group vs 9.3% in the head elevated position. Absolute difference of 13.3%
Limitations: Did not look at emergency department intubation. More experienced intubators used the BUHE positioning, which could confound the reduction in intubation related complications [1].
BUHE or Head Elevated Laryngoscopy Position (HELP) has also been found to
- Improve laryngeal view [2,3]
- Prolong safe apnea time [4]
Note: in patients with possible spinal injuries, one may use reverse trendelenberg (or forego the back up head elevated position)
Core Content
We delve into core content on the esophagus using Rosen’s (8th ed) Chapter 71 and Chapter 77 in Tintinalli (8th ed)
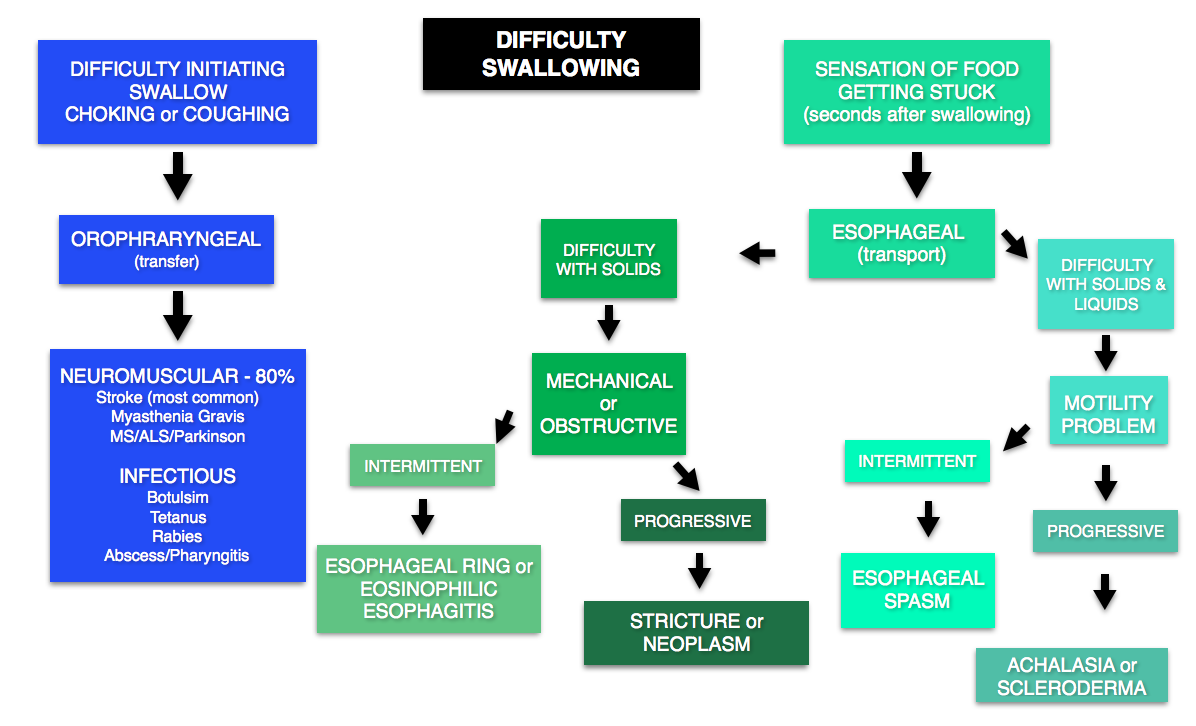
DYSPHAGIA
Emergent conditions may include stroke (most common cause), myasthenia/botulism/or other neuromuscular problems (may also have concomitant respiratory failure). Many causes do not need emergent workup.
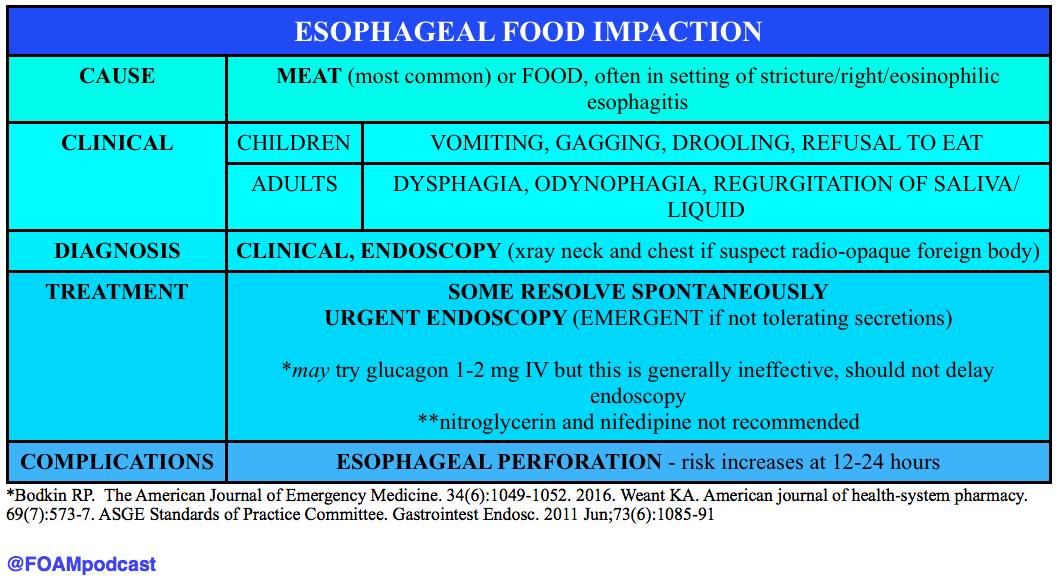
ESOPHAGEAL FOOD BOLUS
Generously Donated Rosh Review Questions
An 87-year-old woman presents to the ED after her caregiver witnessed the patient having difficulty swallowing over the past 2 days. The patient is having difficulty with both solids and liquids. She requires multiple swallowing attempts and occasionally has a mild choking episode. She has no other complaints. Your exam is unremarkable. Which of the following is the most likely cause of her condition?
A. Achalasia
B. Cerebrovascular accident
C. Esophageal neoplasm
D. Foreign body
[accordion]
[toggle title=”Answer” state=”closed”]
B. Cerebrovascular accident. Dysphagia can be divided into two categories: transfer and transport. Transfer dysphagia occurs early in swallowing and is often described by the patient as difficulty with initiation of swallowing. Transport dysphagia occurs due to impaired movement of the bolus down the esophagus and through the lower sphincter. This patient is experiencing a transfer dysphagia. This condition is most commonly due to neuromuscular disorders that result in misdirection of the food bolus and requires repeated swallowing attempts. A cerebrovascular accident (stroke)that causes muscle weakness of the oropharyngeal muscles is frequently the underlying cause. Achalasia (A) is the most common motility disorder producing dysphagia. It is typically seen in patients between 20 and 40 years of age and is associated with esophageal spasm, chest pain, and odynophagia. Esophageal neoplasm (C) usually leads to dysphagia over a period of months and progresses from symptoms with solids to liquids. It is also associated with weight loss and bleeding. Foreign bodies (D) such as a food bolus can lead to dysphagia, but patients are typically unable to tolerate secretions and are often observed drooling. These patients do not have difficulty in initiating swallowing.
[/toggle]
[/accordion]
A 33-year-old man presents with dysphagia to both solids and liquids, with solids being worse than liquids. He describes a sensation of the food getting stuck in his chest. Occasionally, he needs to raise his arms above his head to help food pass into his stomach. His primary care doctor has been treating him for GERD over the previous six months, but his symptoms are getting worse. Which of the following is the most likely diagnosis?
A. Achalasia
B. Diffuse esophageal spasm
C. Schatzki ring
D. Zenker’s diverticulum
[accordion]
[toggle title=”Answer” state=”closed”]
Achalasia This patient most likely has achalasia, which is an esophageal dysmotility disorder due to failure of the lower esophageal sphincter to relax. Dysphagia is the most common symptom. While all patients have dysphagia to solids, only two-thirds have liquid dysphagia. By standing after eating, straightening one’s back, or raising the arms above the head, the esophageal pressure increases, which can help emptying into the stomach. Symptoms usually begin with mild dysphagia in patients who are 20 to 40 years old; symptoms are usually progressive. Diffuse esophageal spasm (B) is a hypermotility disorder causing strong, uncoordinated peristaltic contractions that do not propel food effectively to the stomach. Dysphagia, regurgitation of food, and chest pain are commonly present. The dysphagia is intermittent and does not progress over time. A Schatzki ring (C) is a fibrous band-like structure in the distal esophagus that is the most common cause of dysphagia with solids. Patients typically do not experience difficulty with liquids. Zenker’s diverticulum (D) is an acquired disease that is due to an out-pouching in the mucosa of the pharynx. It typically occurs in individuals older than 50 years and can cause regurgitation, cough, and halitosis from food that becomes stuck in the diverticulum.
[/toggle]
[/accordion]
[accordion]
[toggle title=”What are three common treatments for achalasia?” state=”Closed”]
Nitroglycerin to reduce lower esophageal sphincter tone, endoscopic injection of botulinum toxin into the muscle of the sphincter, and surgical myotomy. Diffuse esophageal spasm (B) is a hypermotility disorder causing strong, uncoordinated peristaltic contractions that do not propel food effectively to the stomach. Dysphagia, regurgitation of food, and chest pain are commonly present. The dysphagia is intermittent and does not progress over time. A Schatzki ring (C) is a fibrous band-like structure in the distal esophagus that is the most common cause of dysphagia with solids. Patients typically do not experience difficulty with liquids. Zenker’s diverticulum (D) is an acquired disease that is due to an out-pouching in the mucosa of the pharynx. It typically occurs in individuals older than 50 years and can cause regurgitation, cough, and halitosis from food that becomes stuck in the diverticulum.
[/toggle]
[/accordion]
References
- Khandelwal et al. Head-elevated Patient Positioning Decreases Complications of Emergent Tracheal Intubation in the Ward and Intensive Care Unit. Anesthesia and Analgesia. Apr 2016.
- Lee et al. Laryngeal exposure during laryngoscopy is better in the 25 degree back-up position than in the supine position. British Journal of Anaesthesia. July 2007.
- Levitan RM, Mechem CC, Ochroch EA, Shofer FS, Hollander JE. Head-elevated laryngoscopy position: improving laryngeal exposure during laryngoscopy by increasing head elevation. Annals of emergency medicine. 41(3):322-30. 2003.
- Ramkumar V, Umesh G, Philip FA. Preoxygenation with 20º head-up tilt provides longer duration of non-hypoxic apnea than conventional preoxygenation in non-obese healthy adults. Journal of anesthesia. 25(2):189-94. 2011. [pubmed]
- Bodkin RP, Weant KA, Baker Justice S, Spencer MT, Acquisto NM. Effectiveness of glucagon in relieving esophageal foreign body impaction: a multicenter study. The American Journal of Emergency Medicine. 34(6):1049-1052. 2016.
- Weant KA, Weant MP. Safety and efficacy of glucagon for the relief of acute esophageal food impaction. American journal of health-system pharmacy : AJHP : official journal of the American Society of Health-System Pharmacists. 69(7):573-7. 2012
- ASGE Standards of Practice Committee, Ikenberry SO, Jue TL, Anderson MA, Appalaneni V, Banerjee S, Ben-Menachem T, Decker GA, Fanelli RD, Fisher LR, Fukami N, Harrison ME, et al. Management of ingested foreign bodies and food impactions. Gastrointest Endosc. 2011 Jun;73(6):1085-91