(ITUNES OR Listen Here)
The Free Open Access Medical Education (FOAM)
The St. Emlyn’s team ran a post on the REVERT trial, which added a new spin to the traditional (and traditionally ineffective) Valsalva maneuver for stable supraventricular tachycardia (SVT). In this post, Dr. Rick Body goes through the trial covering not only the results but also drops pearls on methodology.
- Randomized 433 patients with SVT to one of the following:
- “Modified” Valsalva maneuver: patient sitting up performs Valsalva using a syringe to maintain 40 mm Hg for 15 sec and then placed supine with passive leg raise immediately after procedure (see video)
- “Standard” Valsalva maneuver: patient sitting up performs Valsalva using a syringe to maintain 40 mm Hg for 15 sec while maintaining upright position
- 43% of the patients in modified Valsalva group versus 17% in the standard technique achieved sinus rhythm at one minute yielding an absolute risk reduction of 26.2% (p<0.001) with a number needed to treat of about 4 (3.8).
Core Content – Supraventricular Tachycardia (SVT) and Ventricular Tachycardia (VT)
Tintinalli (7e) Chapter 22; Rosen’s Emergency Medicine (8e) Chapter 79
SVT
Broad term referring to tachycardias originating above the ventricles, including the regular rhythms of sinus tachycardia, AV nodal reentrant tachycardia, AV reentrant tachycardia, and the irregular rhythms of multifocal atrial tachycardia, atrial fibrillation, and some forms of atrial flutter.
Diagnosis: JACC algorithm
Treatment:
- Unstable patients – electrical cardioversion at 0.5-1 J/kg (100J for an adult) + ABCs!
- Stable patients-
- Valsalva maneuver – we like this method of having a patient blow on a syringe. Unfortunately, prior to the REVERT trial, the valsalva maneuver success rate has been documented ~19% [3].
- Adenosine (0.1mg/kg or 6 mg in adult; 2nd dose 0.2 mg/kg or 12 mg in adult, with occasional dose adjustments) – administration can be tricky because of the drug’s short half life, necessitating proximal administration, elevation of the arm, and a quick saline flush afterwards. You can combine the adenosine IN the flush as detailed in this post, meaning no stopcock.
- Calcium channel blockers or beta-blockers (verapamil, diltiazem or even metoprolol, esmolol) – Recently the calcium channel blockers have increased in popularity in the FOAM world and these are Rosenalli approved [4,5].
VT
Diagnosis: Typically wide QRS complex (95% with QRS >120 ms) and fast (150-200 beats per minute).
- SVT with abberency can have a wide complex but this should be treated as VT [4,5] (see this video)
- Monomorphic – complexes have same morphology
- Polymorphic – complexes of various morphologies, associated with poor prognosis [4,5]
Treatment:
- Unstable patients – electrical cardioversion at 0.5-1 J/kg (100J for an adult) + ABCs!
- Stable patients with monomorphic VT–
- Electrical cardioversion
- Procainamide – Level B recommendation for first line treatment of monomorphic VT[6].
- Amiodarone – common in the US but per the AHA guidelines “reasonable in patients with sustained monomorphic VT that is hemodynamically unstable, refractory to conversion with countershock, or recurrent despite procainamide or other agents. (Level of Evidence: C)” [6].
- Note: Dangerous if prolonged QT [6]
- Lidocaine – “may be reasonable” [6]
- Stable patients with polymorphic VT –
- Electrical cardioversion
- Beta-blockers (particularly if ischemic)
- Amiodarone
- Cardiac catheterization if potentially ischemic cause [6]
- Torsades de Pointes – withdraw offending agent, magnesium sulfate IV if “a few episodes” per the AHA
Generously Donated Rosh Review Questions
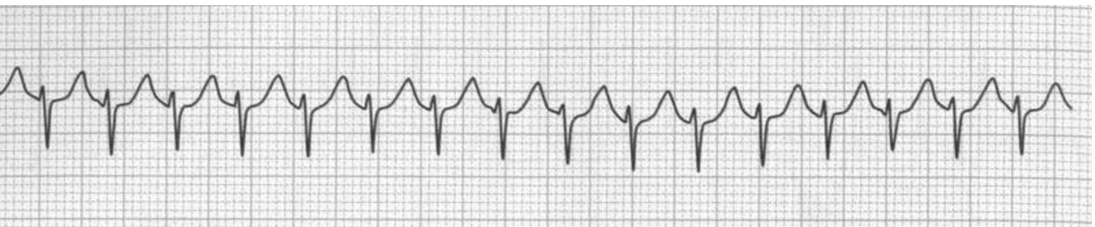
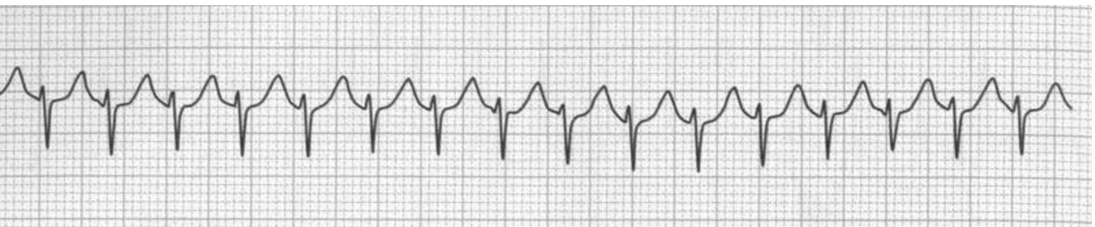
Question 1. A 26-year-old woman presents with dizziness and palpitations. She reports episodes of these symptoms beginning about 1 week ago, which initially only lasted a few minutes. However, for the past two days, she has had about 4 episodes a day which last about 20 minutes each. Her social history is significant for heavy caffeine intake. Her pulse is 166 bpm and her blood pressure is 140/70. Her rhythm strip is seen below. [polldaddy poll=9061960]
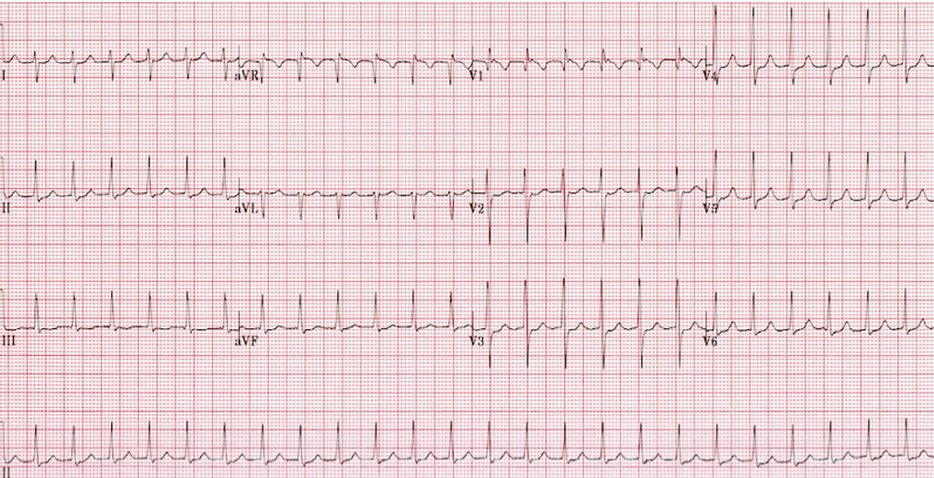
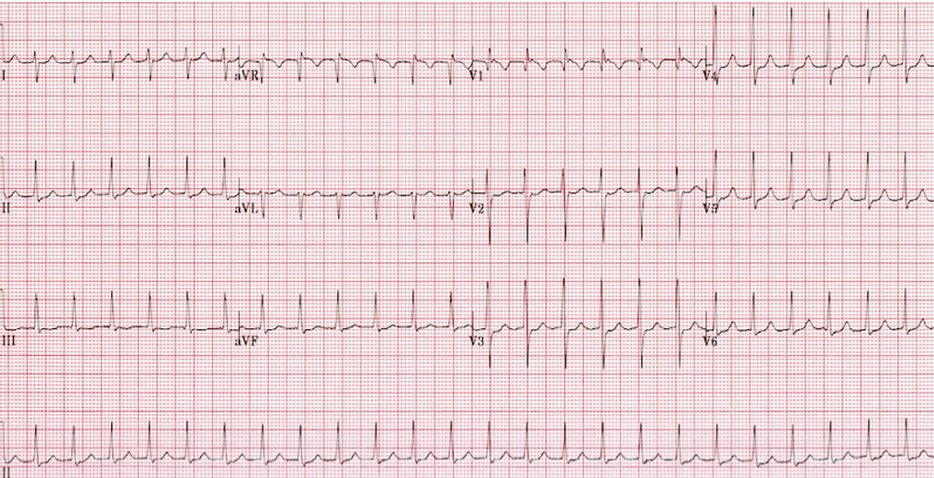
Question 2. A 33-year-old woman with chronic persistent asthma presents with palpitations. Her vital signs are HR 210, BP 118/73, and pulse oxygenation of 97% on room air. An ECG is shown below. [polldaddy poll=9061966]
References:
- Whinnett ZI, Sohaib SM, Davies DW. Diagnosis and management of supraventricular tachycardia. BMJ (Clinical research ed.). 345:e7769. 2012
- Link MS. Clinical practice. Evaluation and initial treatment of supraventricular tachycardia. The New England journal of medicine. 367(15):1438-48. 2012.
- Smith et al. Effectiveness of the Valsalva Manoeuvre for reversion of supraventricular tachycardia. Cochrane Database Syst Rev. 2013 Mar 28;3:CD009502. doi: 10.1002/14651858.CD009502.pub2
- ”Cardiac Rhythm Disturbances.” Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th ed. pp 136-146.
- “Tachyarrhythmias.” Rosen’s Emergency Medicine. 8th ed. Chapter 79.
- Zipes DP, Camm AJ, Borggrefe M et al. ACC/AHA/ESC 2006 Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death. Journal of the American College of Cardiology. 48(5):e247-e346. 2006