The Free Open Access Medical Education (FOAM)
We review a FOAM post by Dr. Matthew MacPartlin on Rollcage Medic on flying after a pneumothorax.
Increases in altitude are accompanied by decreases in pressure that cause the volume of gas to expand (Boyle’s law – pressure and gas volume are inversely associated). As such, gas filled spaces, such as a pneumothorax, may expand during ascent, particularly many thousand meters, as in is the case of aircraft.
- British Thoracic Society (2011) – No commercial flights until full resolution of pneumothorax, confirmed by chest x-ray. They ideally recommend waiting 7 days after resolution of spontaneous pneumothorax and 14 days after resolution of traumatic pneumothorax. The risk of pneumothorax recurrence drops after one year [1].
- An observational paper by Sacco and colleagues report the experience of patients flying after chest tube removal, but before the 7-14 day waiting period and found, in their experience, this was safe [2]
Core Content
Tintinalli (8e) Ch 221, Rosen’s Emergency Medicine (8e) Ch 144.
Generously Donated Rosh Review Questions
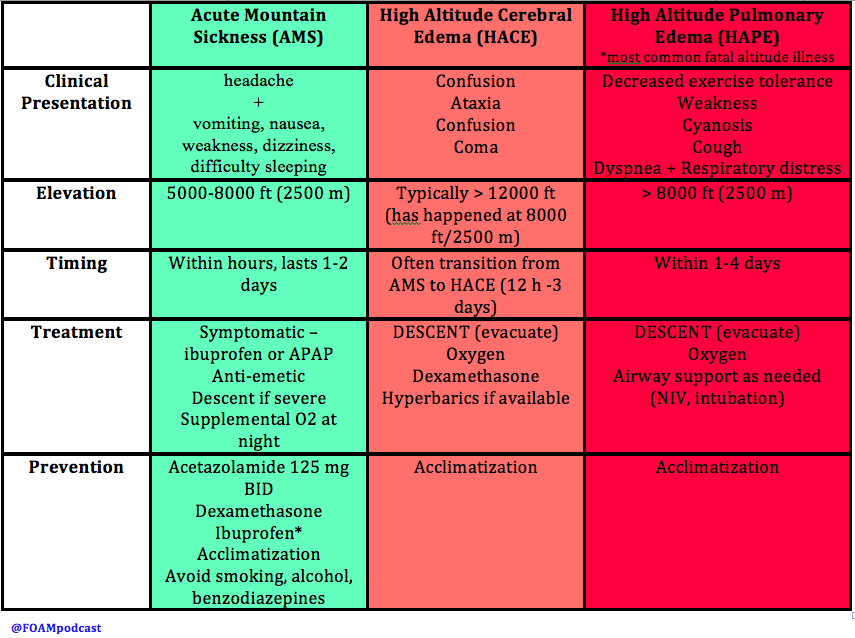
A 20-year-old woman is climbing Mt. Kilimanjaro when she begins developing a headache followed by vomiting. As you begin to assess her, she has a grand mal seizure. Which of the following treatments should immediately be started?
A. Descent and acetazolamide
B. Ibuprofen and dexamethasone
C. Supplemental oxygen and acetazolamide
D. Supplemental oxygen, descent, and dexamethasone
[accordion]
[toggle title=”Answer” state=”closed”]
This patient has developed high-altitude cerebral edema (HACE), a rare but potentially life-threatening form of high-altitude illness. Most cases of HACE are described in ascension past 12 000 feet although it may happen at altitudes as low as 8 200 feet. In HACE, mild altered mental status can rapidly progress to coma in as little as 12 hours. HACE is characterized by global cerebral dysfunction evidenced by headache, fatigue, vomiting, ataxia, confusion, generalized seizures, slurred speech, and focal neurologic deficits. It is a clinical diagnosis although imaging will show cerebral edema. Treatment should start with high-flow oxygen, dexamethasone, and immediate descent. Additionally, if hyperbaric treatment is available, it should be initiated. Ibuprofen (B) and other NSAIDs can be used for prophylaxis prior to ascent as can acetazolamide (A and C).
[/toggle]
[/accordion]
A 32-year-old man complains of dyspnea on exertion and a cough with clear, watery sputum. He has been climbing Mt. Kilimanjaro for 2 days. Other than descent, what treatment can be started immediately?
A. Acetazolamide
B. Albuterol
C. Furosemide
D. Portable hyperbaric chamber therapy
[accordion]
[toggle title=”Answer” state=”closed”]
The patient is suffering from high-altitude pulmonary edema (HAPE) and should be treated with descent from altitude and hyperbaric oxygen therapy. HAPE is the most common fatal manifestation of high-altitude illness. It typically does not develop until the climber has passed 10,000 feet of elevation but it can happen at lower altitudes with heavy activity. The symptoms of HAPE usually begin 2-4 days after arrival at high altitude. Typically, patients experience marked dyspnea on exertion, fatigue with minimal effort, dry cough and difficulty with recovering from exertion. As HAPE progresses, patients will have a cough productive of copious clear secretions and have rales on examination. In severe cases, hemoptysis can develop. Although symptoms may mimic pneumonia or acute cardiogenic pulmonary edema, HAPE should be suspected in the correct clinical scenario. Rapid identification and management is central to preventing morbidity and mortality. The first and most important step in management is descent of the patient. Moderate decreases in altitude (1500 – 3000 feet) can rapidly resolve symptoms. If a hyperbaric chamber is available, it should be employed as simulated descent is just as effective and may be more logistically feasible.

Furosemide (C) is a loop diuretic, which decreases intravascular volume. There is a delay in onset of action and in recent years it has been replaced by pulmonary vasodilators like nifedipine. Additionally, the dehydration associated with furosemide makes it potentially dangerous in these patients. Moreover, HAPE is caused by hypoxia-induced pulmonary vasoconstriction and not from contractility problems of the heart. Acetazolamide (A) is a carbonic anhydrase inhibitor and can be used to treat mild altitude related symptoms like acute mountain sickness (AMS) or to prevent the development of high-altitude illnesses but it is not an appropriate treatment in HAPE. Albuterol (B) plays no role in the treatment of HAPE as bronchospasm is not the problem
[/toggle]
[/accordion]
References
- Ahmedzai S, Balfour-Lynn IM, Bewick T et al. Managing passengers with stable respiratory disease planning air travel: British Thoracic Society recommendations. Thorax. 66(Suppl 1):i1-i30. 2011. [article]
- Sacco F, Calero KR. Safety of early air travel after treatment of traumatic pneumothorax. Int J Circumpolar Health. 2014; 73.
- Cheatham ML, Safcsak K. Air travel following traumatic pneumothorax: when is it safe? Am Surg 1999; 65:1160–1164
- Yaron M, Paterson RD, Davis CB. “High Altitude Medicine.” Chapter 144. Rosen’s Emergency Medicine (8e).
- Hackett PH, Davis CB. “High Altitude Disorders.” Chapter 221. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide.