The Free Open Access Medical Education (FOAM)
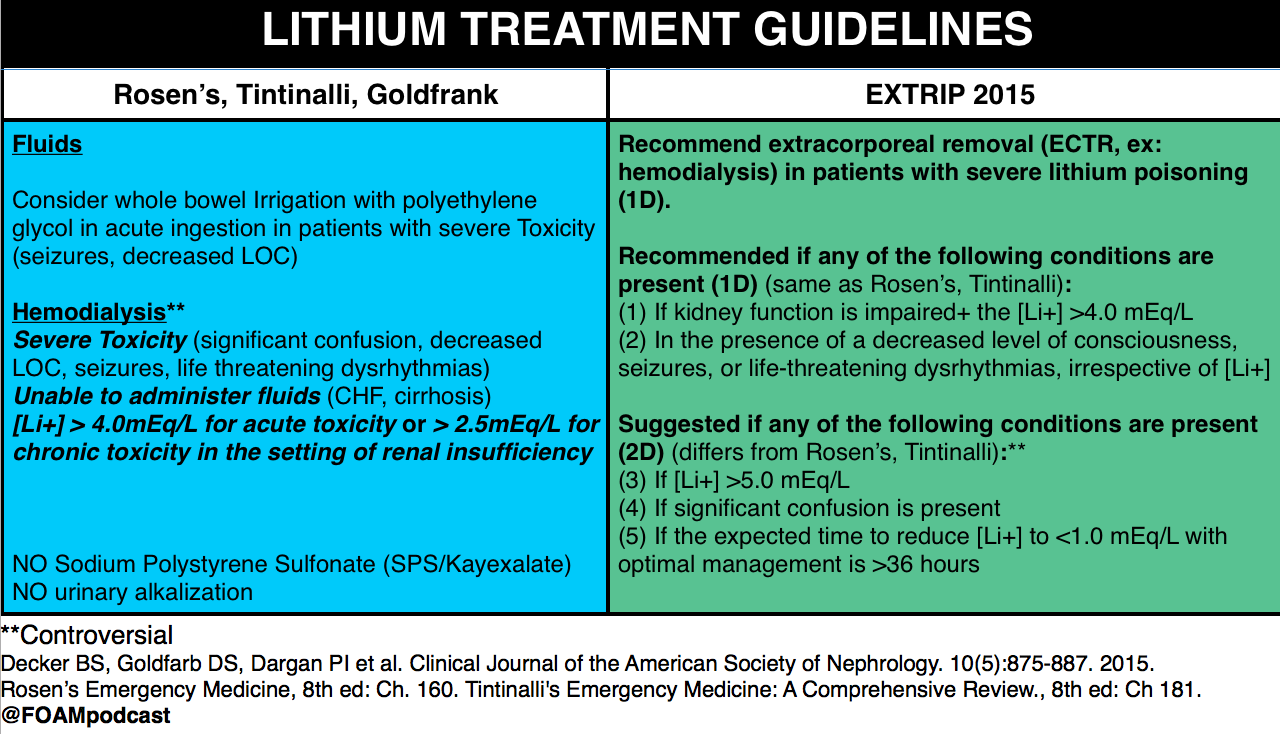
We cover a post from Dr. Josh Farkas on PULMcrit on lithium toxicity. The key message from the post is: a single serum lithium level doesn’t necessitate dialysis, despite a recommendation from the EXTRIP working group to initiate dialysis in patients with a lithium level > 5 mEq/L [1]. Dr. Farkas advocates for aggressive management in asymptomatic patients with chronic lithium toxicity and patients without impaired renal function.
Lithium neurotoxicity does not correlate with serum lithium levels; it depends on the concentration in the CNS.
- The argument is that the neurologic effects, among the most worrisome sequelae of lithium toxicity, results from lithium crossing the blood-brain-barrier (BBB) into the central nervous system (CNS). Thus, in an acute ingestion, patients may have a higher serum lithium level, but given the acuity, the lithium may not cross into the CNS. Conversely, a patient with chronic toxicity may have a mildly elevated serum lithium level but the lithium has had time to cross the BBB into the CNS so more neurotoxicity can result from lower serum lithium concentrations.
Differentiating between acute, chronic, and acute on chronic toxicity is important in management.
- Acute – expect the levels will rise rapidly as the bolus of lithium is absorbed.
- Chronic – expect the levels will not rise rapidly given a lack of lithium bolus.
- Acute on chronic – again, expect levels to rise rapidly and may see more neurotoxicity as some lithium may have passed through the BBB into the CNS.
Core Content
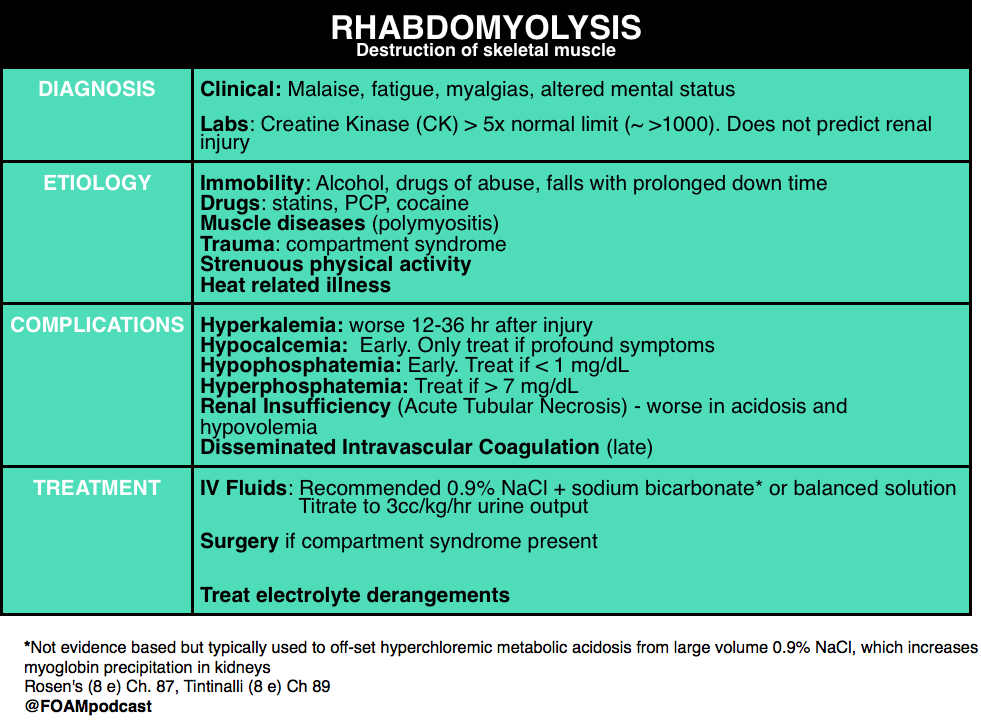
We review rhabdomyolysis using Rosen’s Emergency Medicine (8e) Chapter 160 and Tintinalli’s Emergency Medicine (8e), Chapter 181.
Generously Donated Rosh Review Questions
A 17-year-old man presents to the ED from a correctional facility complaining of general malaise with nausea and vomiting one day after a weightlifting competition. Vital signs are T 37.2°C, BP 100/65 mm Hg, HR 125, and RR 22. Physical exam reveals an uncomfortable, fatigued male who has diffuse muscle soreness. Urinalysis shows 3+ blood without red blood cells. What is the most important next test to direct the acute management of this patient?
A. Creatine kinase assay
B. Electrocardiogram
C. Electrolyte panel with blood urea nitrogen and creatinine
D.Microscopic urinalysis
[accordion]
[toggle title=”Answer” state=”closed”]
B. Electrocardiogram. The patient presents with exercised-induced rhabdomyolysis. Although the causes of rhabdomyolysis are manifold, potential complications are independent of etiology. Of all the complications, hyperkalemia is the most concerning and, undiagnosed, can lead to sudden cardiac death. ECG changes indicative of hyperkalemia are thus critical to identify early in the course of management. Hyperkalemia results from impaired calcium transport with increased intracellular calcium accumulation, cellular necrosis, and expulsion of intracellular contents (including potassium) into the bloodstream. Rhabdomyolysis can also lead to acute tubular necrosis and kidney failure, which will exacerbate developing hyperkalemia by decreasing renal potassium clearance. Hyperkalemia is an immediate life-threatening condition that develops shortly after muscle injury. Absent point-of-care electrolyte analyzers, the most rapid way to screen for hyperkalemia is through an electrocardiogram.
Rhabdomyolysis is not defined by a specific creatine kinase (A) level. But, in general, a serum CK >5 times the upper limit of normal (a threshold that may differ by lab) is considered indicative of rhabdomyolysis. Although kidney injury can occur at any level, higher CKs correlate with an increased likelihood for the development of acute renal failure. In the absence of cerebral or myocardial infarction, a CK >5 times is diagnostic for serious muscle injury. Urinalysis (D) typically shows brownish discoloration with “large” blood on dipstick but few, if any, red blood cells on microscopic evaluation. This occurs because most dipstick tests cannot distinguish myoglobinuria from hematuria or hemoglobinuria. Protein, brown casts, and renal tubular epithelial cells may also be present. Measures of renal function and an electrolyte panel (C) should be obtained in all patients with suspected rhabdomyolysis. But, as mentioned, waiting for results may lead to a delay in the identification of life-threatening complications. In addition to hyperkalemia, hyperphosphatemia and hypocalcemia may also be seen. Additional (though less worrisome) laboratory abnormalities include elevated uric acid and low albumin.
[/toggle]
[/accordion]
One Step Further Question: What is the late complication of rhabdomyolysis associated with thrombocytopenia, hypofibrinogenemia, and an elevated D-dimer?
[accordion]
[toggle title=”Answer” state=”closed”]
Disseminated intravascular coagulopathy may occur and is a result of muscle necrosis with liberation of activating substances from injured cells.
[/toggle]
[/accordion]
- References:
- 1. Decker BS, Goldfarb DS, Dargan PI et al. Extracorporeal Treatment for Lithium Poisoning: Systematic Review and Recommendations from the EXTRIP Workgroup. Clinical Journal of the American Society of Nephrology. 10(5):875-887. 2015.
- 2. “Chapter 160. Lithium.” Rosen’s Emergency Medicine. 8th edition.
- 3. “Chapter 181. Lithium.” Tintinalli’s Emergency Medicine: A Comprehensive Review. 8th edition.
- 4. Grellar H. “Chapter 72. Lithium.” Goldfrank’s Toxicology. 10th edition.
- 5. “Chapter 127. Rhabdomyolysis. Rosen’s Emergency Medicine. 8th edition.
- 6. “Chapter 89. Rhabdomyolysis.” Tintinalli’s Emergency Medicine: A Comprehensive Review. 8th edition.

One thought on “Episode 57 – Lithium Toxicity & Rhabdomyolysis”
Comments are closed.