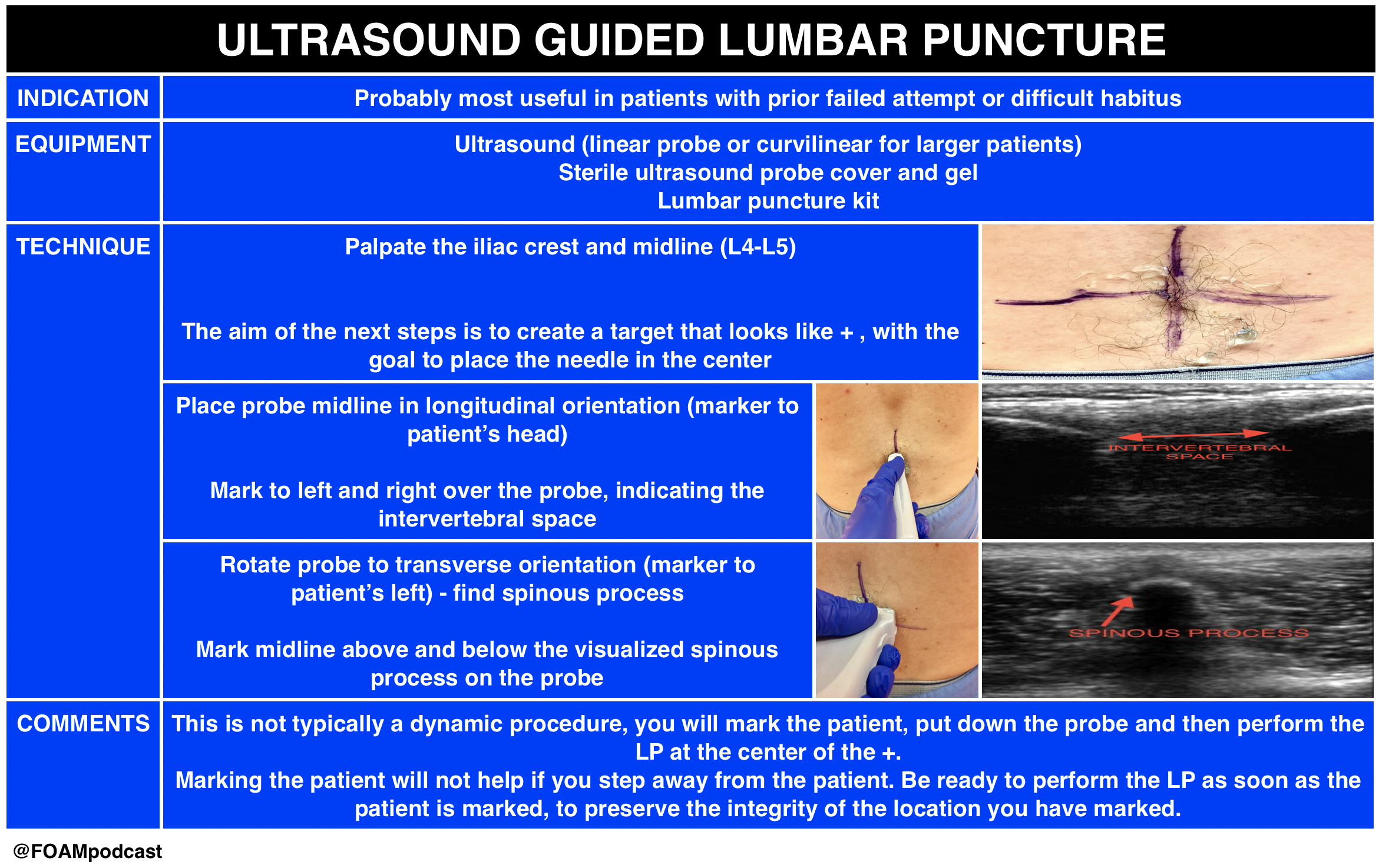
Ultrasound is gaining popularity in assisting lumbar punctures (LPs). We review this technique as well as Free Open Access Medical Education (FOAM) from the following sites: 5 Min Sono, Sinai EM, and PEM pearls from ALiEM.
- This technique is likely most helpful in difficult patients. A recent study demonstrated 27% absolute increase in first attempt success using ultrasound in infants <6 months old undergoing LP; however, the success rate in both arms was abysmal with only 57% success rate in the ultrasound arm.
- Core Content
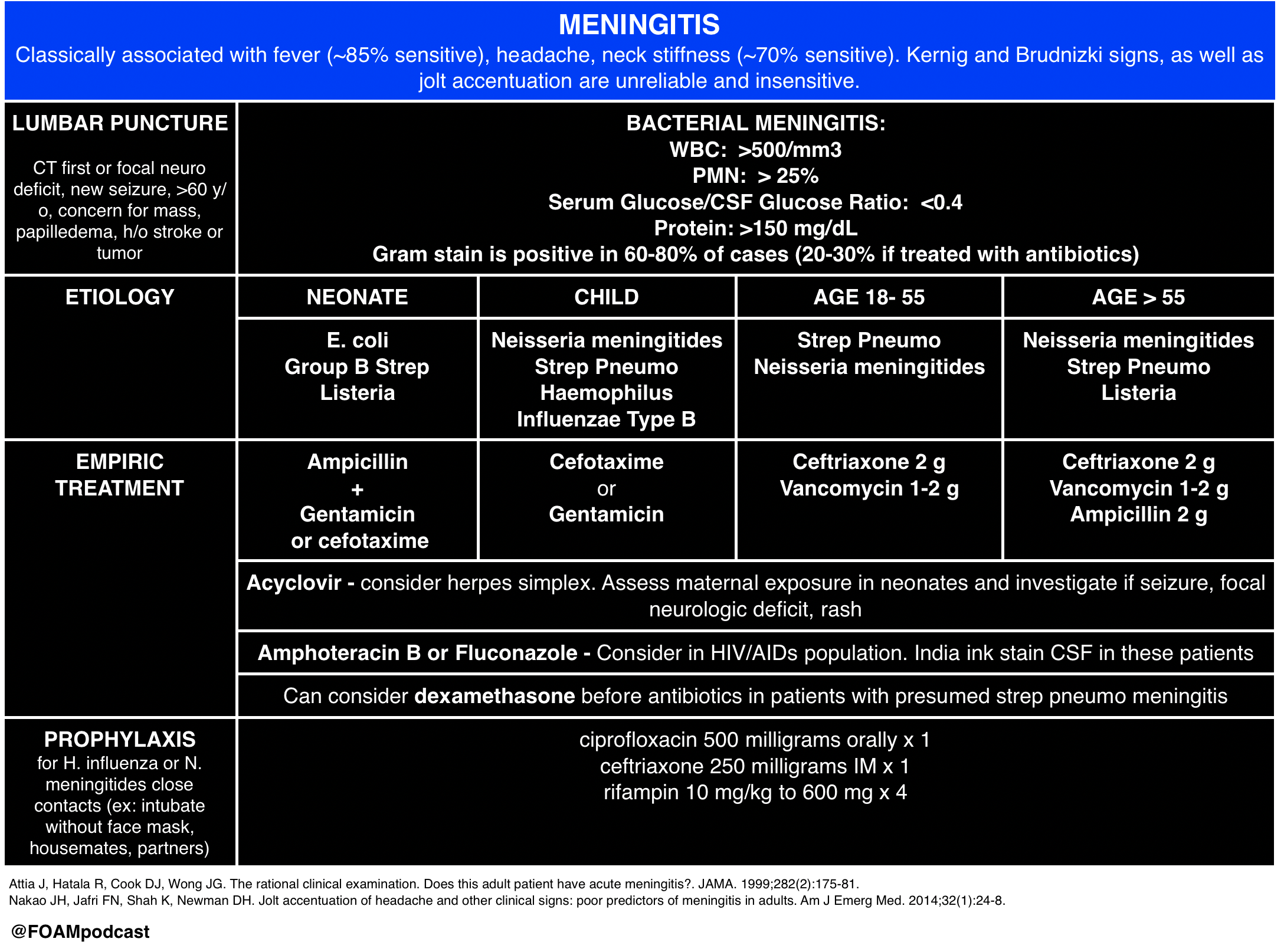
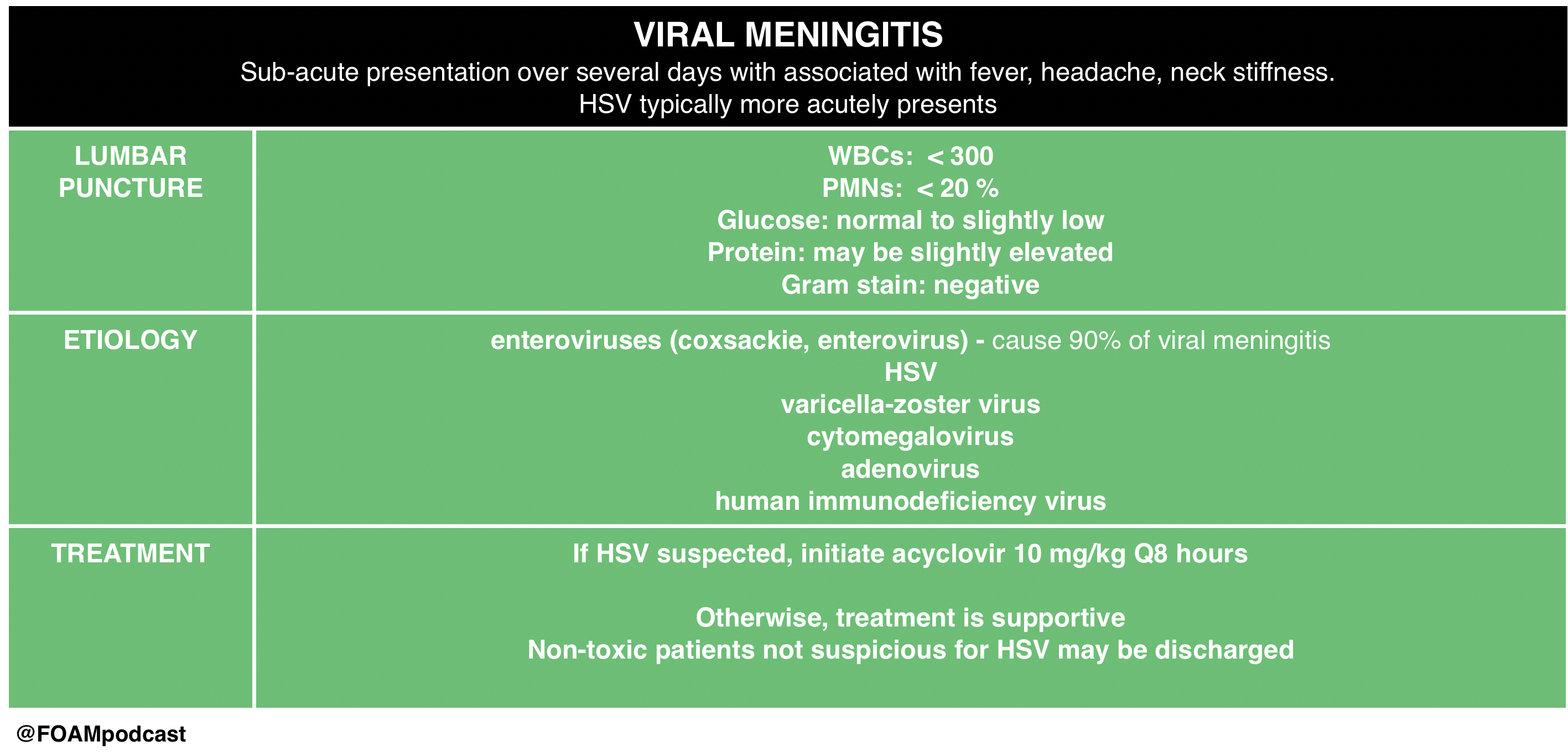
We then delve into core content on meningitis, encephalitis, and antiNMDA receptor encephalitis using Rosen’s Chapter 109 and Tintinalli’s Chapters 117 and 174 as a guide.
Rosh Review Emergency Board Review Questions
A 40-year-old man with HIV presents with two weeks of progressive headache, malaise, and fever. On examination, he has mild nuchal rigidity, confusion, and a temperature of 38.2oC. Cerebrospinal fluid analysis shows a white blood cell count 360 cells/mL with a monocyte predominance, glucose 28 mg/dL, and protein 220 mg/dL. What is the treatment of choice?
A. Acyclovir
B. Amphotericin B
C. Ceftriaxone
D. Vancomycin
[accordion]
[toggle title=”Answer” state=”closed”]
B. Amphotericin B . Cryptococcal meningoencephalitis is an opportunistic infection that occurs primarily in patients with advanced AIDS, although it can be seen in immunocompromised transplant patients as well. The majority of HIV-related cases occur when the CD4 count is < 100 cells/mm3. Patients present with progressive headache, nausea, malaise, and fever over the course of 1 – 2 weeks. Examination findings are typical for meningitis and include altered mental status, photophobia, and fever. Meningismus is less commonly seen. Presentations can be subtle and a high index of suspicion is needed for diagnosis. A CT scan of the brain is indicated if there are signs of increased intracranial pressure or focal neurologic deficits. Lumbar puncture should be performed with careful measurement of the opening pressure. Cerebrospinal fluid will show a mildly elevated white blood cell count with a monocyte predominance, decreased glucose, and mildly elevated protein. However, in some cases the cerebrospinal fluid will only show minor, if any, abnormalities. Cryptococcal antigen testing of the CSF is nearly 100% sensitive and specific. India ink staining will show budding organisms. Treatment of choice is intravenous amphotericin B in addition to oral flucytosine for 14 days followed by an 8 week course of oral fluconazole. Acyclovir (A) is used in the treatment of herpes meningoencephalitis. Ceftriaxone (C) and vancomycin (D) are indicated in the treatment of bacterial meningitis.
[/toggle]
[/accordion]
A previously healthy 18-year-old woman presents to the emergency department with complaints of fever, headache, and neck stiffness. She is accompanied by her sister, who expresses concern because the patient seems suddenly confused and cannot remember what she did yesterday. After you administer empiric intravenous antibiotics, which of the following is the next best step?
A. Chest X-ray
B. Complete blood count with differential
C. Lumbar puncture
D. Urinalysis
[accordion]
[toggle title=”Answer” state=”closed”] C. Lumbar puncture. Meningitis is an inflammation of the tissues surrounding the brain and spinal cord (meninges) and may be of infectious (bacterial, viral, or fungal) and various other etiologies. The classic clinical manifestations include nuchal rigidity, fever and altered mental status. Patients often present with headache as well. All patients with suspected meningitis should have lumbar puncture (LP) to evaluate the cerebrospinal fluid (CSF) unless this procedure is contraindicated. There are no absolute contraindications to LP. Relative contraindications include patients with evidence of increased intracranial pressure, thrombocytopenia, bleeding diathesis or spinal epidural abscess. Acute bacterial meningitis is a medical emergency and left untreated or treated late is almost universally fatal. Treatment involves addressing systemic complications and initiating empiric antibiotic therapy as soon as possible.
Up to half of patients with pneumococcal meningitis may have evidence of pneumonia on chest X-ray (A), but this is not part of the initial workup of patients with suspected meningitis. Complete blood count with differential (B) is often ordered in the workup for bacterial meningitis and generally shows increased white blood cell count, but is not as important to order initially as an LP. Urinalysis (D) is generally not a helpful test in the diagnosis of meningitis and therefore not recommended in the workup for patients with suspected bacterial meningitis.
[/toggle]
[/accordion]
References:
- Attia J, Hatala R, Cook DJ, Wong JG. The rational clinical examination. Does this adult patient have acute meningitis?. JAMA. 1999;282(2):175-81.
- Nakao JH, Jafri FN, Shah K, Newman DH. Jolt accentuation of headache and other clinical signs: poor predictors of meningitis in adults. Am J Emerg Med. 2014;32(1):24-8.
- Neal JT, Kaplan SL, Woodford AL, Desai K, Zorc JJ, Chen AE. The Effect of Bedside Ultrasonographic Skin Marking on Infant Lumbar Puncture Success: A Randomized Controlled Trial. Ann Emerg Med. 2016.
Faust- you’re nuts. Champagne tap is about the skill of the provider – nontraumatic tap. No red cells. White cells are out of your control and actually what you’re looking for. One is not to be faulted for finding pathology