Apple Podcasts , Spotify, Listen Here
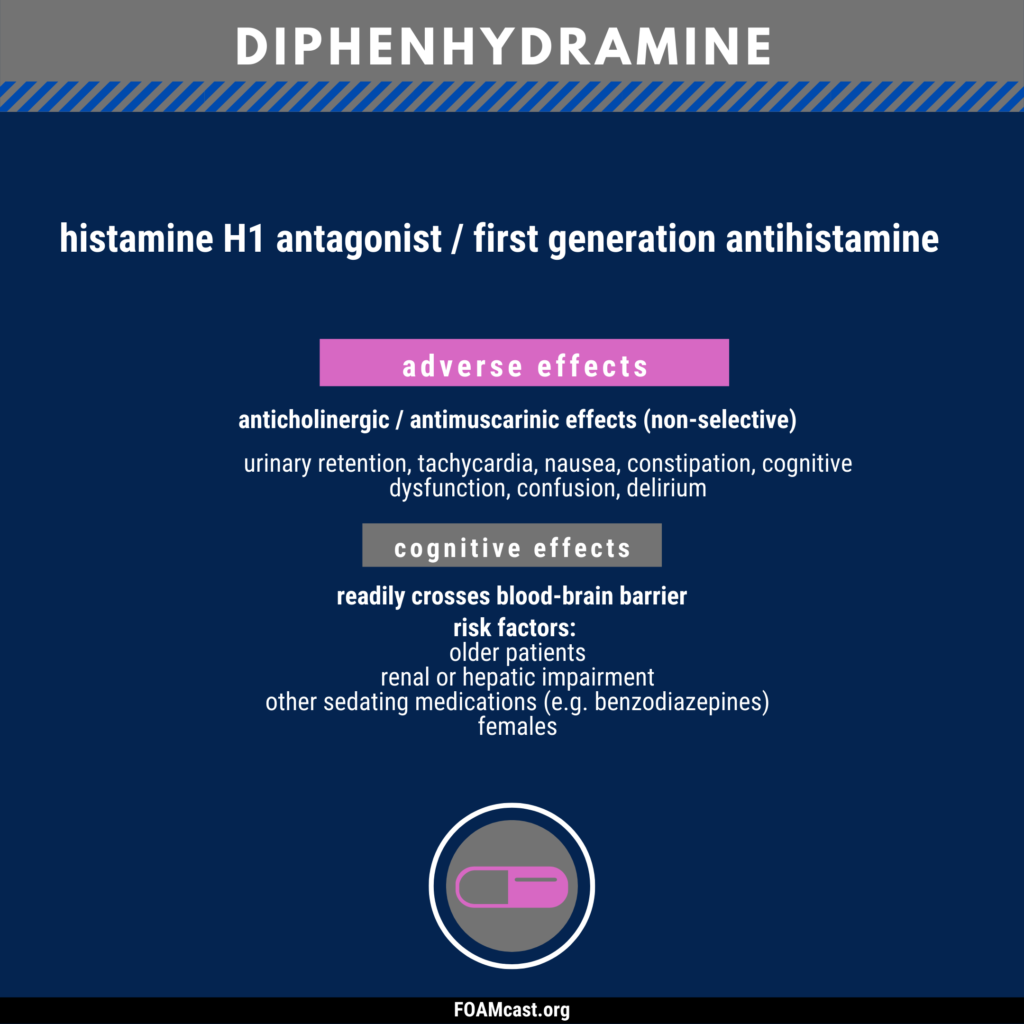
Diphenhydramine and other first-generation antihistamines are ubiquitous in medicine cabinets across the globe. Clinicians commonly recommend or administer diphenhydramine (Benadryl) for a variety of diseases – anaphylaxis, allergic reactions, urticaria, benign headaches/migraines, and as a sleep aid. However, professional societies have recommended against many of these indications for decades and, in other cases, there are safer alternatives. For more reading and references, see this article in ACEPnow.

For more in-depth reviews: Podcast on anaphylaxis and podcast on urticaria
Love this review! I have been consciously limiting my use of diphenhydramine but still find it useful in 2 situations:
1. Agitated patient with contraindications to antipsychotics, benzos, and ketamine: This is still my go-to in patients with prolonged QTc who have history of mania and potential for benzodiazepine abuse, and/or already maxed out their dose of the other classes. Admittedly a small proportion of patients, but we still see them.
2. Patient needing local anesthetic but intolerant of lidocaine: Diphenhydramine is a good local anesthetic and I’ve had many patients who had no response to lidocaine but had substantial improvement in pain with local injection of diphenhydramine.