(ITUNES OR Listen Here)
The Free Open Access Medical Education (FOAM)
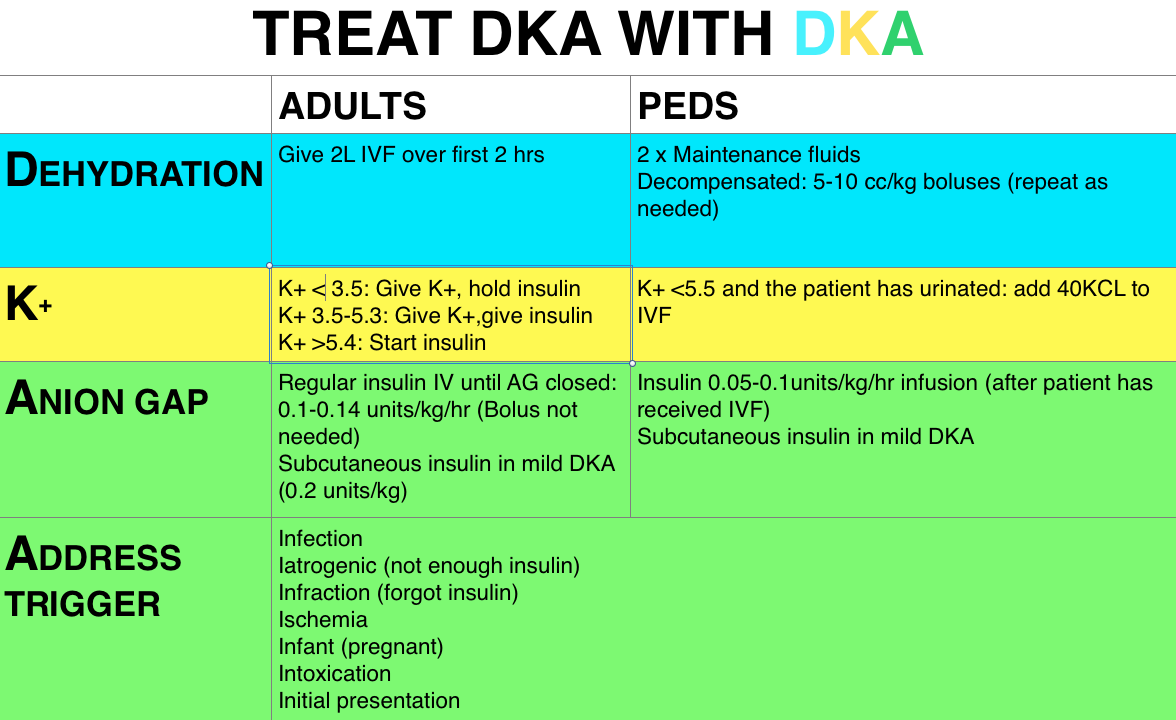
We review a post on Pediatric DKA from Dr. Anton Helman’s Emergency Medicine Cases.
Pearls from this episode:
- Fluids come first in DKA but you may not need as much as you think. They recommend only using fluid boluses, and even then a baby bolus of 5-10 cc/kg, in the hypotensive decompensated patients, coupled with frequent re-assessments. Other patients can get up to twice maintenance of 0.9% NaCl.
- No insulin bolus for pediatric patients, ever.
- Cerebral edema is the most dreaded complication of DKA and seems to be associated with severe presentations, young children (<5), or DKA as the presentation of diabetes. Treatment related factors such as administration of an insulin bolus or sodium bicarbonate may also contribute. The role of fluids (particularly over-aggressive fluids) is less clear [1-3].
- Management of cerebral edema: ABCs, Elevate head of the bed 30 degrees, Mannitol 0.5-1g/kg IV over 20min AND/OR hypertonic (3%) NaCl 5-10cc/kg IV over 30min
The Bread and Butter
We cover hyperglycemia including diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS). We do this based on osen’s Emergency Medicine, Chapter 126 (8th ed) and Tintinalli, Chapter 222 (7th ed). But, don’t just take our word for it. Go enrich your fundamental understanding yourself.
Diabetic Ketoacidosis
Diagnosis – glucose >250 mg/dL, pH <7.3, bicarbonate <18, anion gap >10
Workup – evaluate electrolytes (particularly potassium) and potential triggers for DKA.
Treatment – fluid resuscitation is initial intervention as these patients are typically 4-6 L down. In adults we hold insulin treatment until we know the patient’s serum potassium, as these patient’s are depleted secondary to osmotic diuresis. Further, the patient’s serum potassium may be falsely elevated by acidosis. Insulin may be started once the potassium is >3.5 (with potassium replacement if <5.3). We do not bolus pediatric patients but the ADA guidelines and Rosenalli state we do not need the insulin bolus in adults either [4-6]. The use of subcutaneous insulin in DKA is popular amongst pediatric patients and growing in popularity in adults [7,8].
Hyperosmolar Hyperglycemic State (HHS)
Diagnosis – elevated serum glucose (often >600 mg/dL), serum osmolar >315-320 mOsm/kg. Patient’s may have a concomitant acidosis or ketosis, but this is often less profound than in DKA.
Workup – ascertain why the patient ended up in HHS – whether it was a mobility issue or polypharmacy (diuretic, lithium, etc). Check osmolality and for DKA.
Treatment – these patients are often severely dehydrated (>8 Liters). Start with volume resuscitation and add an insulin infusion (0.1 units/kg/hr).
Generously Donated Rosh Review Questions
1. A 43-year-old man presents with altered mental status. His vital signs are HR 113, BP 143/63, T 98.9°F and blood glucose of 750 mg/dl. During your evaluation he has a brief generalized tonic-clonic seizure. [polldaddy poll=8904849]
Answers
1. This patient presents with signs and symptoms consistent with hyperglycemic hyperosmolar state (HHS) and intravenous fluids should be given aggressively early in management. HHS is a syndrome characterized by dehydration, hyperglycemia, hyperosmolarity and altered mental status. Patients may present with confusion, lethargy, seizures, focal neurologic deficits or frank coma. Pathophysiologically, decreased insulin (or insulin action) leads to gluconeogenesis and increased circulating glucose levels. This in turn draws fluid from the intracellular space into the intravascular space. The resultant osmotic diuresis leads to profound intravascular dehydration, electrolyte abnormalities and hyperosmolarity. Typically, patients will have a blood glucose >600 mg/dl and an osmolarity >350 mOsm/L. Blood urea nitrogen and creatinine are usually elevated. Initial management focuses on supportive care and aggressive fluid resuscitation. Patients with HHS are estimated to be 5-10 liters behind. In addition to fluid administration, electrolyte repletion is paramount.
2. A 45-year-old man presents with altered mental status. On arrival, his finger stick is 35 mg/dL. He is given dextrose leading to the return of a normal mental status. On history, he reports he may have accidentally taken extra medication. Which of the following medications requires prolonged observation in the hospital?
- Glipizide
- Metformin
- Novolog
- Sitagliptin
In most adults, symptomatic hypoglycemia occurs when glucose levels reach 40 to 50 mg/dL. Glipizide is a sulfonyurea oral hypoglycemic drug. This class of medication is associated with hypoglycemic episodes through their action as an insulin secretagogue. In a sulfonylurea overdose, patients should be observed for 24 hours. When the etiology is unclear, laboratory testing including renal function is indicated. In situations without large ingestions, patients may be discharged if no additional episodes of hypoglycemia occur after an observation period. In cases of severe, prolonged or recurrent episodes of hypoglycemia from sulfonylureas, additional therapy with octreotide as an inhibitor of insulin release is indicated.
References:
- Glaser NS, Wootton-Gorges SL, Buonocore MH, et al. Subclinical cerebral edema in children with diabetic ketoacidosis randomized to 2 different rehydration protocols. Pediatrics. 2013;131(1):e73–80. doi:10.1542/peds.2012-1049.
- Glaser N, Barnett P, McCaslin I, et al. Risk factors for cerebral edema in children with diabetic ketoacidosis. The Pediatric Emergency Medicine Collaborative Research Committee of the American Academy of Pediatrics. N Engl J Med. 2001;344(4):264–9. doi:10.1056/NEJM200101253440404.
- Lawrence SE, Cummings E a, Gaboury I, Daneman D. Population-based study of incidence and risk factors for cerebral edema in pediatric diabetic ketoacidosis. J Pediatr. 2005;146(5):688–92. doi:10.1016/j.jpeds.2004.12.041.
- Diabetic Emergencies : New Strategies For An Old Disease.
- Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic crises in adult patients with diabetes. Diabetes Care. 2009;32(7):1335–43. doi:10.2337/dc09-9032.
- Goyal N, Miller JB, Sankey SS, Mossallam U. Utility of initial bolus insulin in the treatment of diabetic ketoacidosis. J Emerg Med. 2010;38(4):422–7. doi:10.1016/j.jemermed.2007.11.033.
- Umpierrez GE, Cuervo R, Karabell A, Latif K, Freire AX, Kitabchi AE. Treatment of diabetic ketoacidosis with subcutaneous insulin aspart. Diabetes Care. 2004;27(8):1873–8. Available at: http://www.ncbi.nlm.nih.gov/pubmed/15277410. Accessed July 17, 2014.
- Umpierrez GE, Latif K, Stoever J, et al. Efficacy of subcutaneous insulin lispro versus continuous intravenous regular insulin for the treatment of patients with diabetic ketoacidosis. Am J Med. 2004;117(5):291–6. doi:10.1016/j.amjmed.2004.05.010.
Fantastic podcast! I am amazed by the production quality and engaging banter.
One point that I think is very important for pediatric DKA that I’m not sure came across is that fluid bonuses should ONLY be given in patients in shock (which is rare). All mild and moderate cases (the vast majority of peds DKA cases) should not get boluses as it is thought boluses of fluid may increase the risk of cerebral edema. Keep up the great work!
Fantastic podcast! I am amazed by the production quality and engaging banter.
One point that I think is very important for pediatric DKA that I’m not sure came across is that fluid bonuses should ONLY be given in patients in shock (which is rare). All mild and moderate cases (the vast majority of peds DKA cases) should not get boluses as it is thought boluses of fluid may increase the risk of cerebral edema. Keep up the great work!
Rosen’s does not recommend insulin infusions on all patients with HHS. Neither Rosen’s nor your podcast mentions hypernatremia as a problem to worry about. Is this not a problem in people? I certainly see it in my patients (dogs and cats) and it is often a cause for concern since rapid correction of hypernatremia may lead to cerebral edema.
Just listened to episodes 29 and 30 on the way to work. Loved them!
Rosen’s does not recommend insulin infusions on all patients with HHS. Neither Rosen’s nor your podcast mentions hypernatremia as a problem to worry about. Is this not a problem in people? I certainly see it in my patients (dogs and cats) and it is often a cause for concern since rapid correction of hypernatremia may lead to cerebral edema.
Just listened to episodes 29 and 30 on the way to work. Loved them!