iTunes or Listen Here
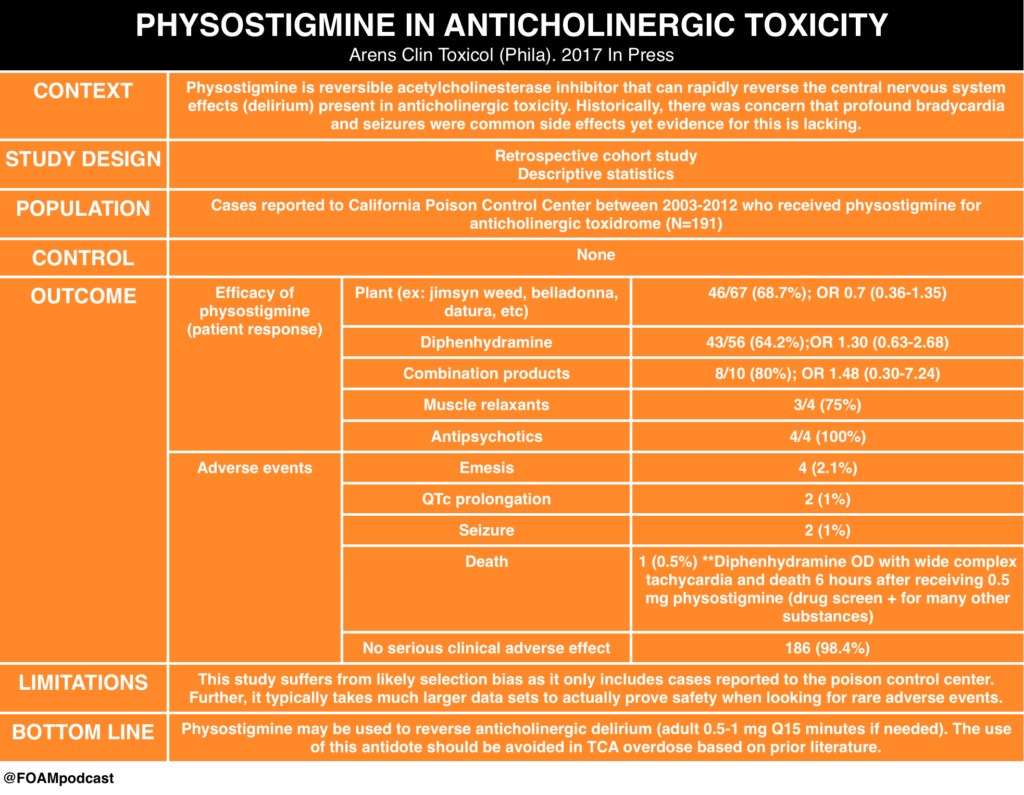
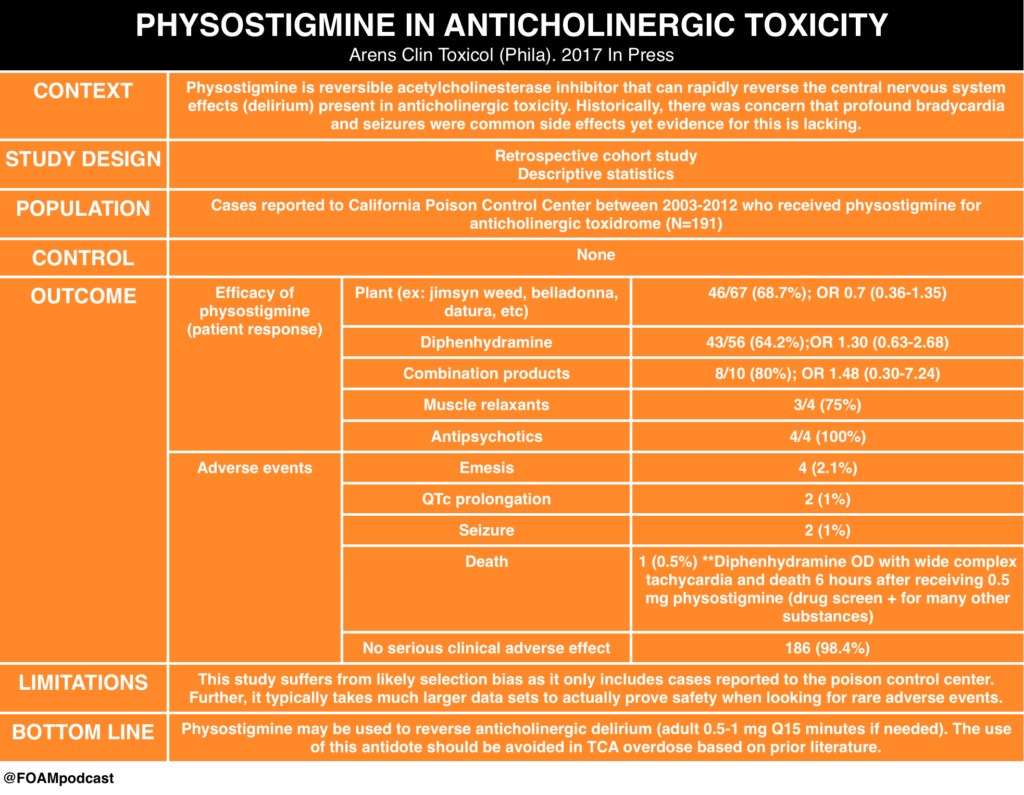
We review this blog post by Bryan Hayes, an ED pharmacist (@PharmERToxGuy), on the use of physostigmine in anticholinergic toxicity.
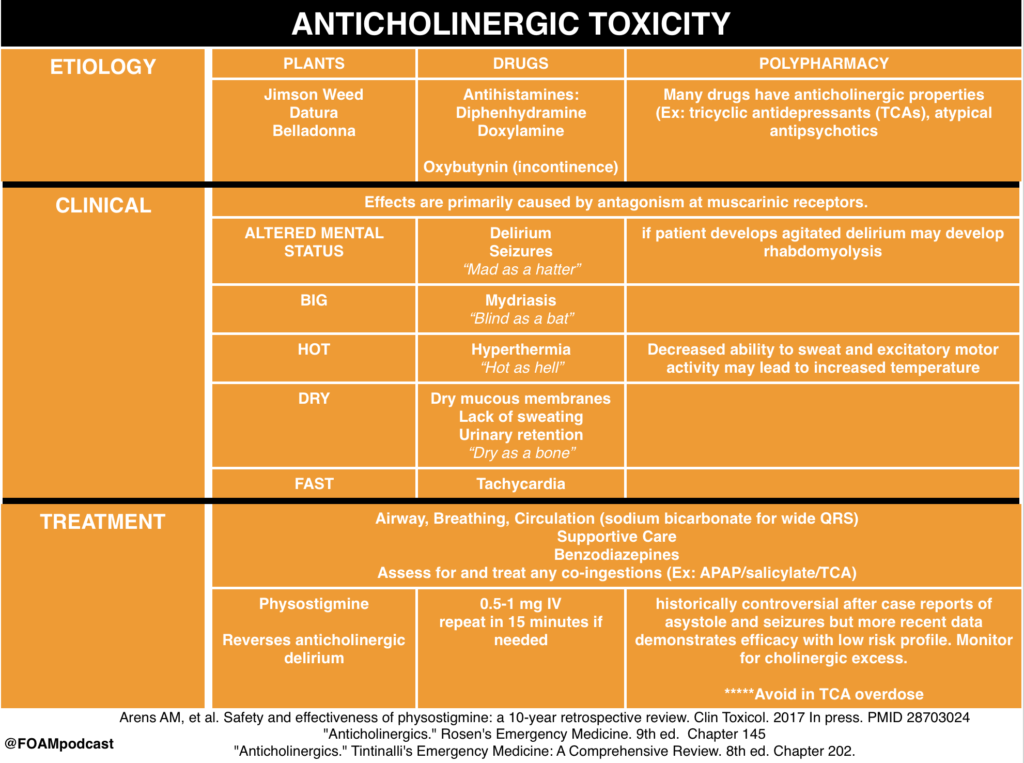
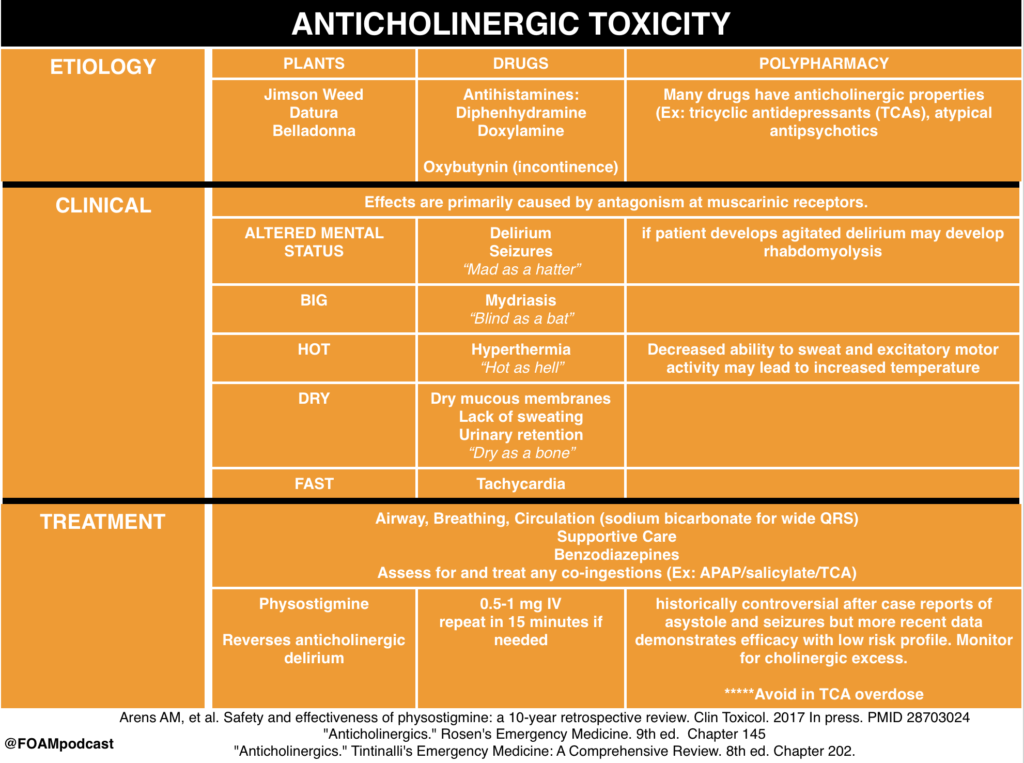
We review core content on anticholinergic toxicity using Rosen’s Emergency Medicine (9th ed), Tintinalli’s Emergency Medicine (8th ed) and Goldrank’s Toxicology as guides.
Rosh Review Emergency Board Review Questions
A 27-year-old man is brought to the ED by EMS after being found wandering in the street. His BP is 155/70, HR 115, T 37.5°C, RR 16, pulse ox 99% on room air, and finger stick glucose 98. On exam, the patient is confused with mumbling speech. His pupils are 7 mm and nonreactive. His face is flushed. Mucous membranes and skin are dry. Which of the following toxidromes is this patient exhibiting?
A. Anticholinergic
B. Cholinergic
C. Sedative-hypnotic
D. Sympathomimetic
[accordion]
[toggle title=”Answer” state=”closed”]
A. Anticholinergic Toxidrome refers to a constellation of physical findings that can provide important clues in a toxic ingestion. This patient exhibits an anticholinergic toxidrome. Anticholinergics are widely available as over-the-counter cold preparations and sleep aids (diphenhydramine, chlorpheniramine, doxylamine). They also are the basis of the toxicity of jimsonweed. Anticholinergics competitively inhibit acetylcholine in the central and peripheral nervous systems. This classic toxidrome is often described by the phrase “mad as a hatter (altered mental status), blind as a bat (mydriasis), red as a beet (flushed skin), hot as a hare (dry skin due to inability to sweat), dry as a bone (dry mucous membranes).” Other findings include tachycardia, delirium, seizures, and hallucinations. Treatment is mainly supportive with benzodiazepines for agitation and seizures, and cooling for temperature reduction. Gastric decontamination (whole-bowel irrigation or gastric lavage) is often recommended due to the delay in gastric emptying caused by anticholinergics. The use of physostigmine, a reversible cholinesterase inhibitor that will increase synaptic acetylcholine, is controversial and should be administered only in consultation with a toxicologist.
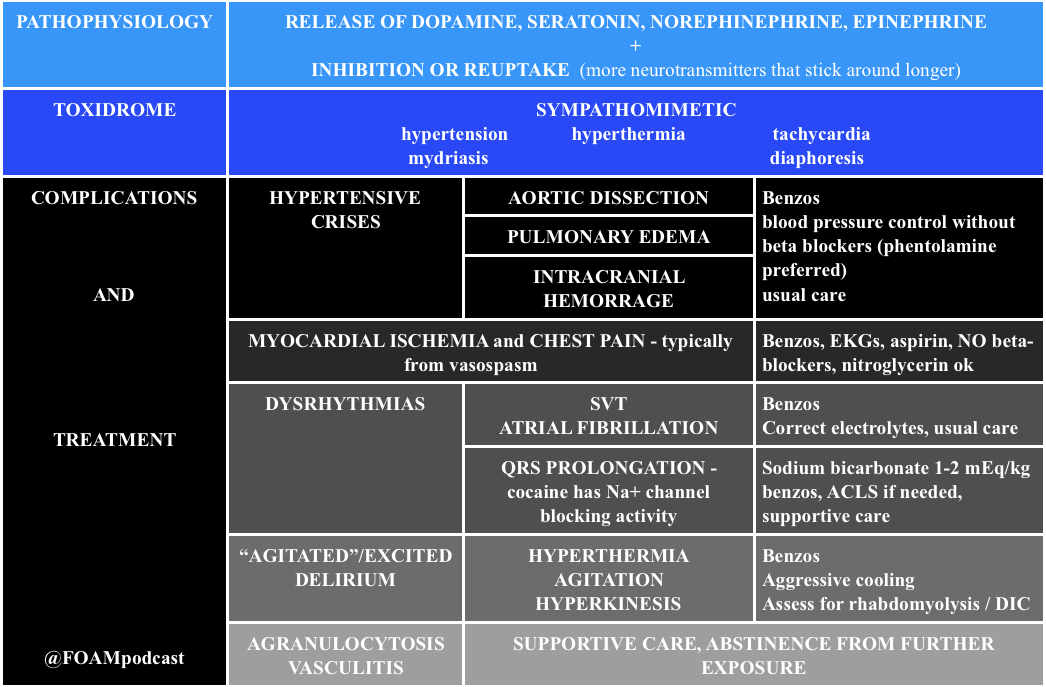
The cholinergic toxidrome (B) is characterized by the mnemonics SLUDGE (salivation, lacrimation, urination, defecation, GI upset, emesis) or DUMBBELS (defecation, urination, miosis, bronchospasm, bronchorrhea, emesis, lacrimation, salivation) and occurs after exposure to organophosphates or carbamates. The sedative-hypnotic toxidrome (C) is seen with benzodiazepines and barbiturates. Clinically, patients exhibit central nervous system and respiratory depression. The sympathomimetic toxidromes (D) can occur after ingestion of cocaine, amphetamines, or decongestants. It typically presents with delirium, paranoia, tachycardia, hypertension, hyperpyrexia, diaphoresis, mydriasis, seizures, and hyperactive bowel sounds. Sympathomimetic and anticholinergic toxidromes are frequently difficult to distinguish. The key difference is that sympathomimetics are associated with diaphoresis, whereas anticholinergics cause dry skin.
[/toggle]
[/accordion]
A 22-year-old man is brought into the Emergency Department by Emergency Medical Services with altered mental status. He is an agitated man and mumbling incoherent words. His pupils are 6 mm and reactive to light. His axillae are dry. His heart rate is 115 beats/minute and temperature is 101.6 oF. Which of the following is a complication of the antidote used in the treatment of this condition?
A. Asystole
B. Bladder retention
C. QT-interval prolongation
D. Respiratory depression
[accordion]
[toggle title=”Answer” state=”closed”]
Asystole. The mnemonic for the anticholinergic toxidrome is blind as a bat (mydriasis), red as a beet (vasodilation leading to flushing), hot as a hare (hyperthermia), dry as a bone (dry skin and mucosa), mad as a hatter (visual or auditory hallucinations, agitation, and mumbling or incoherent speech), bloated as a toad (ileus and urinary retention), and the heart runs alone (tachycardia). Additionally, anticholinergic toxicity can cause orthostatic hypotension (especially in the elderly), picking behavior, and can lead to seizures, coma, and even death. There are multiple anticholinergic medications, including tricyclic antidepressants, antihistamines, antiparkinson medications, antipsychotics, antispasmodics, belladonna alkaloids, skeletal muscle relaxants, and mydriatics. Antihistamine overdose is the most common cause of anticholinergic toxicity. Treatment is supportive with IV hydration. If the ingestion occurred within one hour, GI decontamination with activated charcoal is reasonable. Benzodiazepines are used for significant agitation and seizures. Good temperature control should be achieved with antipyretics and active cooling is essential. For wide complex tachyarrhythmias, treatment is with sodium bicarbonate. The antidote is physostigmine, a reversible acetylcholinesterase inhibitor. There is, however, a risk of profound bradycardia, seizures, and asystole in patients with widened QRS complexes. This risk is minimal if there is a pure anticholinergic syndrome without concomitant sodium channel blockade, but this is unfortunately not always known. Since the most common cause of anticholinergic toxicity is from diphenhydramine overdose (which causes sodium channel blockade), physostigmine should only be used with the assistance of a medical toxicologist.
[/toggle]
[/accordion]
References:
- Arens AM, et al. Safety and effectiveness of physostigmine: a 10-year retrospective review. Clin Toxicol. 2017 Jul 13:1-7. [Epub ahead of print] PMID 28703024
- “Anticholinergics.” Rosen’s Emergency Medicine. 9th ed. Chapter 145
- “Anticholinergics.” Tintinalli’s Emergency Medicine: A Comprehensive Review. 8th ed. Chapter 202.