In this episode we highlight key articles in Emergency Medicine that came out, thus far, in 2018.
D’souza et al. Effects of prophylactic anticholinergic medications to decrease extrapyramidal side effects in patients taking acute antiemetic drugs: a systematic review and meta-analysis Emerg Med J. 2018;35(5):325-331.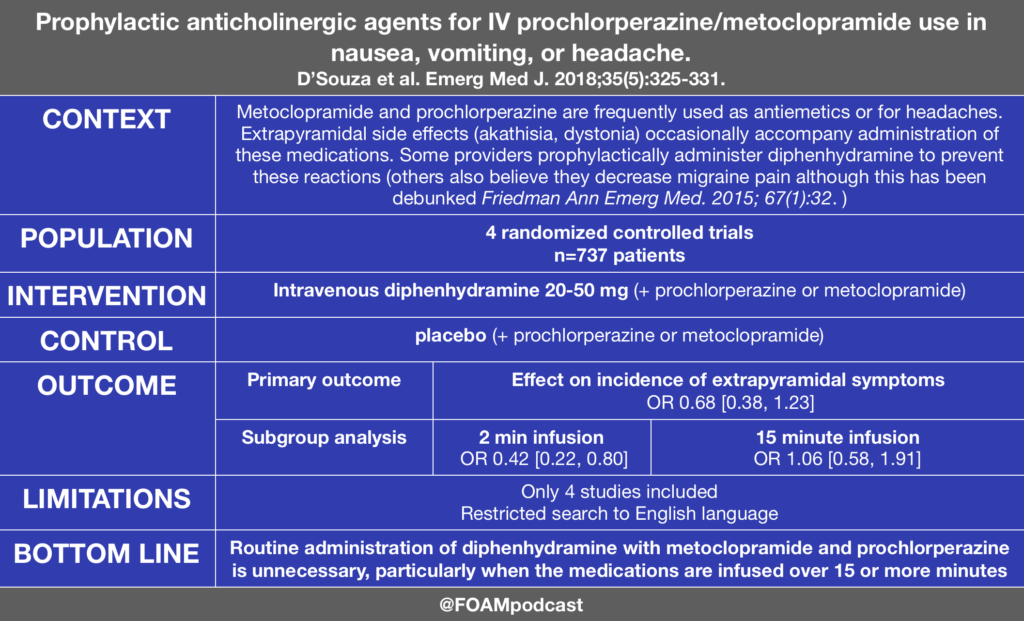
Driver et al. Effect of Use of a Bougie vs Endotracheal Tube and Stylet on First-Attempt Intubation Success Among Patients With Difficult Airways Undergoing Emergency Intubation: A Randomized Clinical Trial. JAMA. 2018;319(21):2179-2189.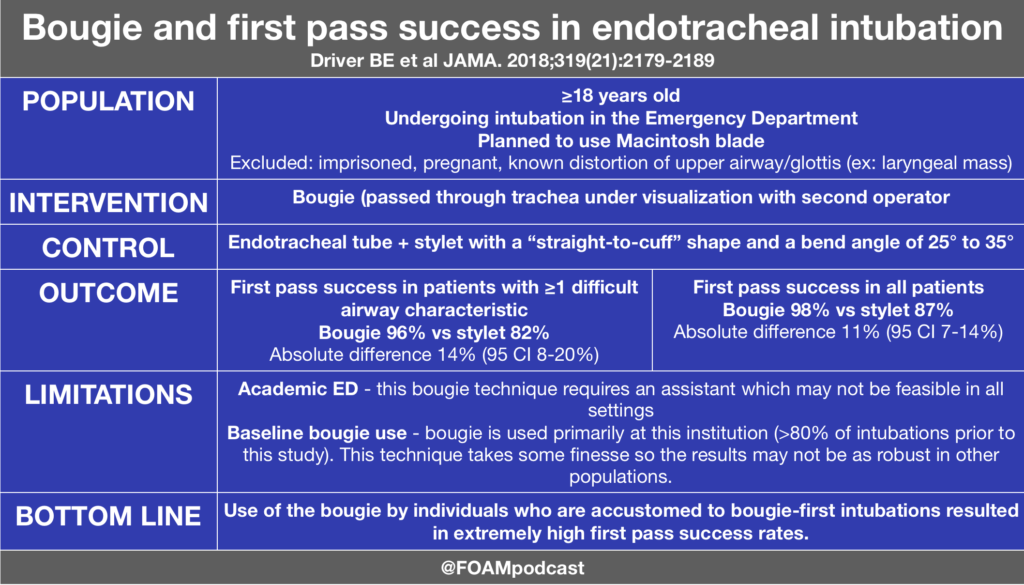 Atkinson PR, Milne J, Diegelmann L, et al. Does Point-of-Care Ultrasonography Improve Clinical Outcomes in Emergency Department Patients With Undifferentiated Hypotension? An International Randomized Controlled Trial From the SHoC-ED Investigators. Ann Emerg Med. 2018; In press.
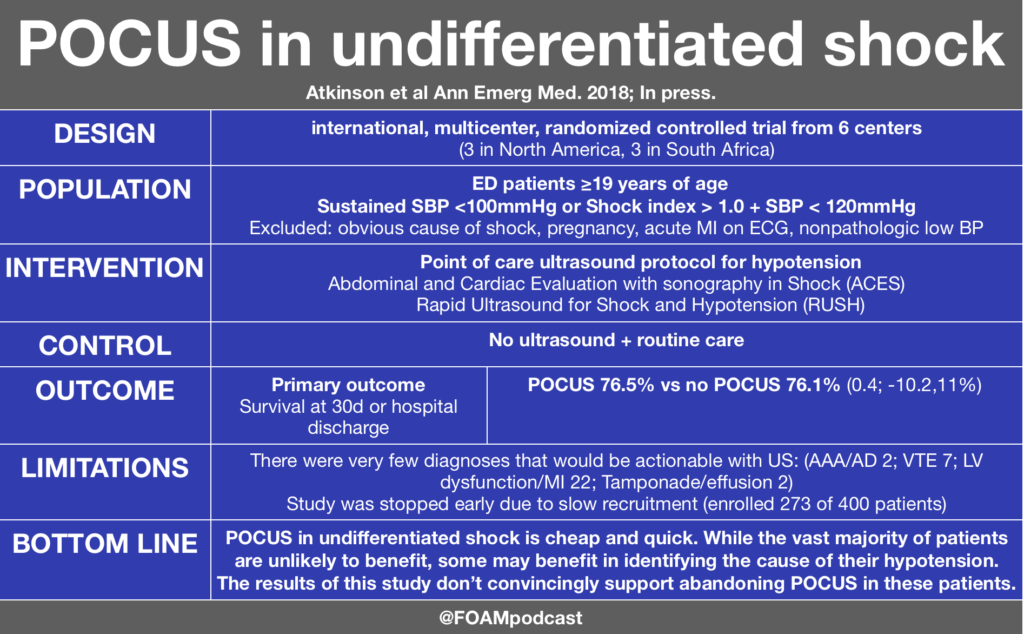
Atkinson PR, Milne J, Diegelmann L, et al. Does Point-of-Care Ultrasonography Improve Clinical Outcomes in Emergency Department Patients With Undifferentiated Hypotension? An International Randomized Controlled Trial From the SHoC-ED Investigators. Ann Emerg Med. 2018; In press.
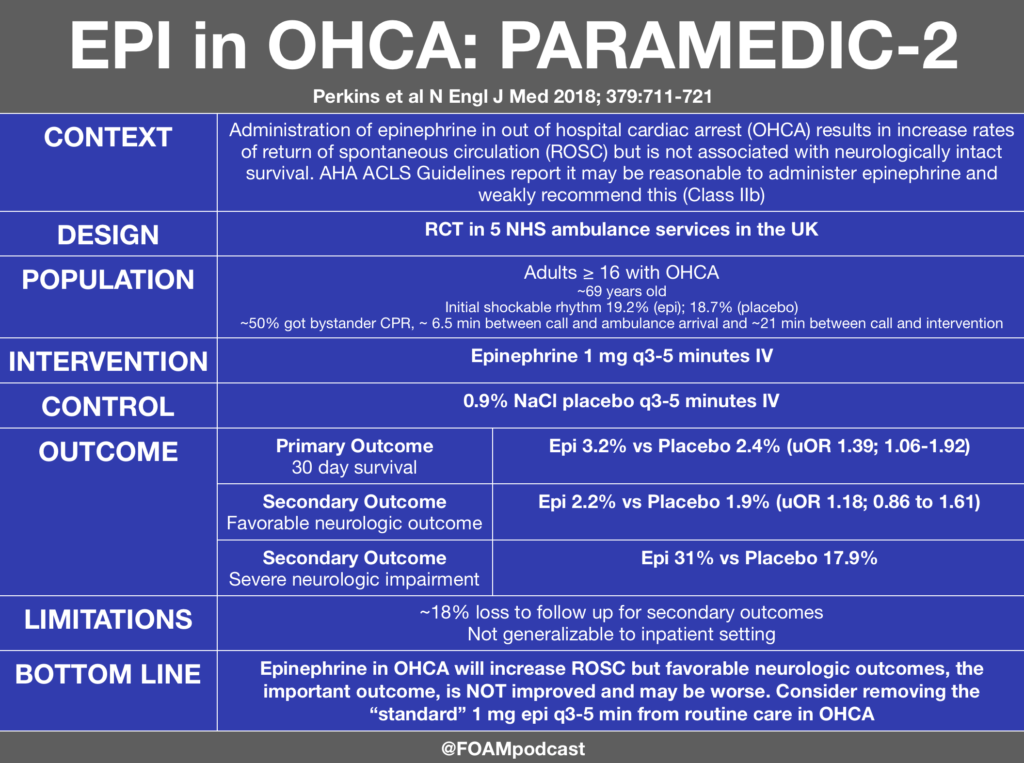
Perkins GD et al. A Randomized Trial of Epinephrine in Out-of-Hospital Cardiac Arrest. N Engl J Med 2018; 379:711-721
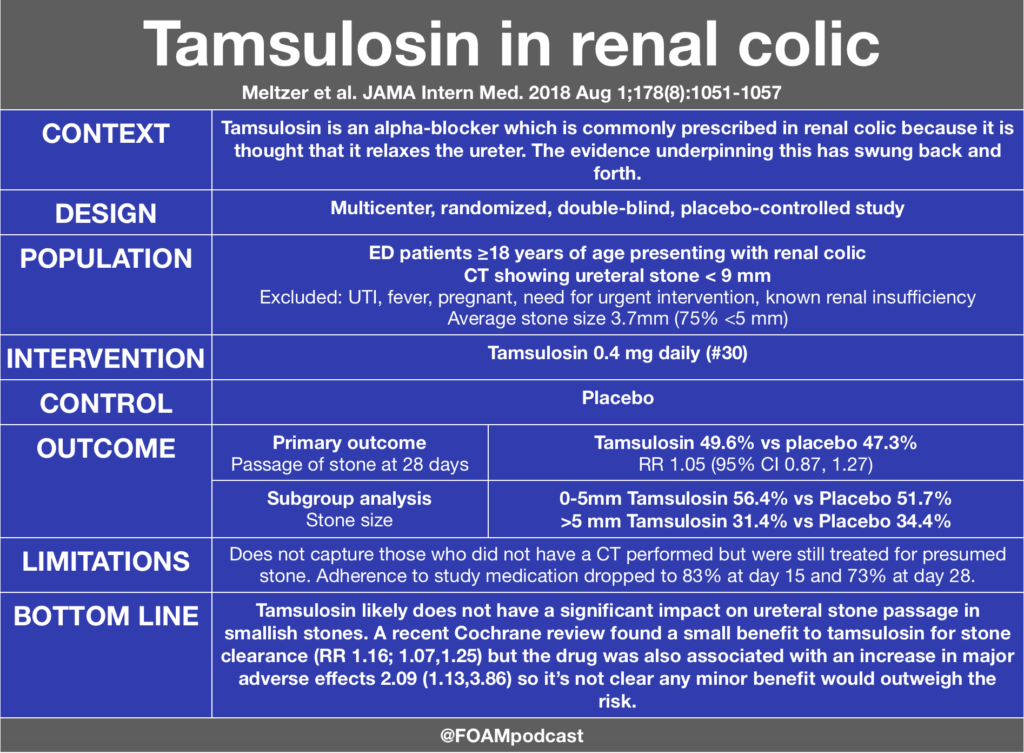
Meltzer et al. Effect of Tamsulosin on Passage of Symptomatic Ureteral Stones: A Randomized Clinical Trial. JAMA Intern Med. 2018 Aug 1;178(8):1051-1057
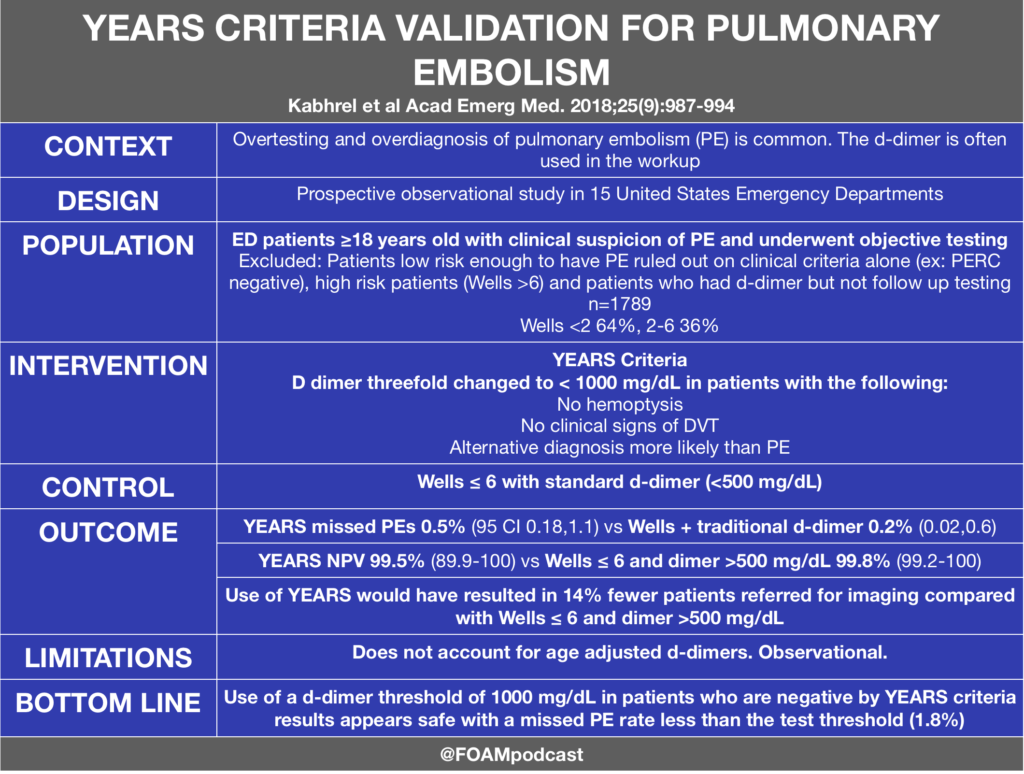
Kabrhel et al Multicenter Evaluation of the YEARS Criteria in Emergency Department Patients Evaluated for Pulmonary Embolism. Acad Emerg Med. 2018;25(9):987-994
Thanks, very useful!
Great literature, thank you so much for sharing!
Years Criteria suffers a similar problem with Wells Criteria where application of the test would be dependent on clinical gestalt – does paitient have a PE or is there another more likely cause. I like the idea of it reducing CTPA’s, but time will tell if it translates to clinical usefullness in Aussie EDs.
Agree – I think that implementation in the right population (and by the right providers) is important. If there is a likely alternative explanation, those are patients that I often (depending on the patient) wouldn’t work up for PE so I wouldn’t order a dimer to begin with. In the United States, alot of people get sent down this pathway (maybe they have pleuritic chest pain that is probably MSK but they don’t feel comfortable with that) so a dimer to 1 is more appropriate than a dimer of 0.5. On a note about Wells,I actually like knowing that I can dimer a patient in whom i have no alternative diagnosis, is tachycardic, and has a history of prior DVT/PE (Wells 6)….i.e. the higher risk patients, but not technically “high risk’ Wells>6 patients. From surveying US docs, it seems that few dimer patients who satisfy only the PE most likely diagnosis criteria and they go straight to CTPA (even though the Wells may be 3-4). – LW