(ITUNES OR Listen Here)
The Free Open Access Medical Education (FOAM)
This week we cover posts from the Wessex ICS site, The Bottom Line, which is an excellent source for breakdown of recent and important trials. This site is great for reviews of high impact trials in critical care. We cover their post on a systematic review of peripheral pressor complications and then we delve into a recent prospective trial by Cardenas-Garcia and colleagues that came up at SMACC.
The Bottom Line on the Loubani paper
- Systematic review of the literature 1946-Jan 2014 (does not include most recent trial)
- Outcome – local tissue injury or extravasation: 325 separate events, 318/325 peripheral pressors
- Signal that distal lines are not ideal for running pressors: 204 events (local tissue injury) were distal to the antecubital fossa/popliteal fossa (90% of events)
- Signal that duration of pressors running peripherally may impact likelihood of adverse event. Increasing number of events were reported at the 6-12 hour mark (n=9) then 12-24 hour (n=18) and then almost all >24 hour
- Single arm consecutive study of ICU patients
- ICU fellows and attendings determined if peripheral pressors were warranted and then initiated the following protocol:
- Vein diameter >4 mm measured with ultrasonography and PIV confirmed with US before pressors started
- Upper extremity only, contralateral to the blood pressure cuff
- IV size 20 gauge or 18 gauge
- No hand, wrist, or antecubital fossa PIV access position
- Blood return from the PIV access prior to VM administration
- Assessment of PIV access function q 2h as per nursing protocol
- Immediate alert by nursing staff to the medical team if line extravasation, with prompt initiation of local treatment
- 72 hours maximum duration of PIV access use
- N=734 patients
- 19/783 peripheral vasopressor administrations with infiltration of site (2%) with no events of local tissue injury
The take home: If a patient needs vasopressors, you can start them through a good, proximal peripheral IV. Sometimes patient or situation factors delay central lines, this doesn’t mean it needs to delay patient’s therapy. Know what to do in the event of infiltration (see this EMCrit post).
Core Content
Tintinalli (7e) Chapter 24
Panchal et al – Phenylephrine bolus dosing in peri-intubation period
Central line technique from Dr. Reuben Strayer – Wire through catheter vs wire through needle
Generously Donated Rosh Review Questions
1.[polldaddy poll=8996471]
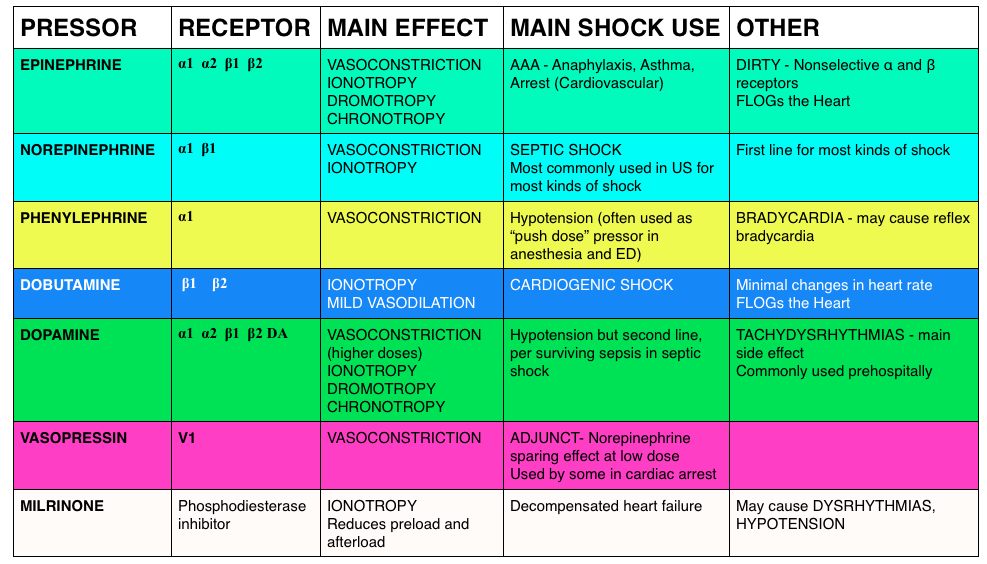
Answer. C. Norepinephrine is considered the vasopressor of choice for treatment of septic shock. Norepinephrine acts primarily as an α-adrenergic agonist, causing vasoconstriction that results in an increase in blood pressure. It also has β-adrenergic properties, which causes an increase in cardiac output and heart rate. The combination of α-adrenergic and β-adrenergic properties benefits patients who have septic shock. Norepinephrine also has a short duration of action, which allows for rapid adjustment of dosing in response to changes in a patient’s hemodynamic status. Dopamine (A) was once widely used in the treatment of septic shock, but studies have shown that it has no advantage over norepinephrine and its use is associated with a higher death rate. Epinephrine (B) has both α-adrenergic and β-adrenergic properties and has a greater affinity for alpha- and beta-receptors than norepinephrine. Its use is associated with a higher rate of cardiac dysrhythmias and a decrease in splanchnic blood flow. Phenylephrine (D) is a pure α-adrenergic agent that causes vasoconstriction and impairment of tissue blood flow throughout the body, most notably in the splanchnic circulation.