(ITUNES OR LISTEN HERE)
The Free Open Access Medical Education (FOAM)
We review Dr. Scott Weingart’s episode 133 on pre-hospital REBOA (resuscitative endovascular balloon occlusion of the aorta). Weingart interviews Dr. Gareth Davies about the encounter, underscoring the increasing use of REBOA.
For a quick REBOA refresher, check out Episode 121.
REBOA (Review of REBOA) – First described in 1954 in the Korean War, this is a form of hemorrhage control below the level of the chest without having to do a thoracotomy with aortic cross clamping, which has sparse mortality benefit and can be dangerous to providers. Most of the REBOA literature is from swine models and case-series, although there are currently larger trials underway.
- Outline of procedure – Obtain arterial access through the common femoral artery, pass a vascular sheath, float a balloon catheter to the appropriate section of the aorta, and inflate the balloon to occlude blood flow. The aorta is divided into three zones so that balloon occlusion is performed in Zone 1 for abdominal injuries or Zone 3 for pelvic injuries, while Zone 2 is a proposed no-occlusion zone.
The Bread and Butter
Rosen’s Chapter 46, 134 and Tintinalli Chapter 260.
What DOES the spleen do?
Answer: More than most appreciate. The spleen filters the blood, removing abnormal or old red blood cells (RBCs), debris, and antibody coated bacteria from the bloodstream. It also serves as a reservoir for RBCs and platelets and synthesizes antibodies, opsonins, etc.
Splenic Trauma – EAST Guidelines (their podcast)
Diagnosis – suspect spleen trauma clinically, with hypotension, left upper quadrant abdominal pain, or even minimal trauma, especially after infectious mononucleosis.
- CT with IV contrast (hemodynamically stable patients). While FAST and DPL can detect peritoneal free fluid, they can’t detect subcapsular bleeds.
- Unstable patients – operating room versus interventional radiology
Grading – 1 is 1 (<1 cm laceration depth), 3 is 3 (>3 cm laceration depth). Everything else is somewhere in between. Higher grades typically result in more aggressive interventions. Historically these get operative intervention
- Grade 1: < 1 cm laceration depth or<10% subcapsular hematoma
- Grade 2: 1-3 cm laceration or 10-50% subcapsular
- Grade 3: > 3 cm laceration depth or >50% subcapsular hematoma
- Grade 3 or higher should be considered for angiography with embolization (Level II, III – EAST)
- Grade 4: partially devascularized spleen or contrast blush
- Grade 5: a very battered, devascularized spleen
There’s slightly more to spleen grading, check out this post from Dr. McGonigal
Trivia: The punctate extravasation sometimes seen on angiogram after blunt trauma?
Answer: The Seurat Spleen (pubmed), named after the pointillist painter.
Treatment –
- Unstable patients: Operating room or Angiographic Intervention (IR) (Level II – EAST)
- Note: Board exam? Send the patient to the OR. In reality, there is some practice variation. Many would still argue the patient belongs in the OR, some places have combined OR/IR suites, and some opt for IR.
- Post splenectomy patients will need immunizations for the encapsulated bacteria
- Stable patients: Nonoperative management, which often comprises in-hospital monitoring, serial abdominal exams and hematocrits, etc is becoming increasingly common as first line for higher grade splenic injuries. The key here is that the team must be able to take the patient to the OR or IR should the situation change. Angioembolization has also gained momentum as management
Post-Splenectomy Sepsis (Review)– Most common in the first years after splenectomy and in children.
Presentation – Patients may present with a vague flu-like illness or gastroenteritis but may go on to develop septic shock, DIC, and multiorgan dysfunction. In addition, meningitis without overwhelming infection or shock is a common presentation of pneumococcal infection in asplenic patients.
Etiology – encapsulated bacteria (Streptococcus pneumoniae, Haemophilus influenza, and Neisseria meningitidis), capnocytophaga canimorsus (dog bites), and parasites such as babesiosis (endemic in New England), malaria, and ehrlichiosis.
Management – Labs, blood cultures, antibiotics (typically ceftriaxone)
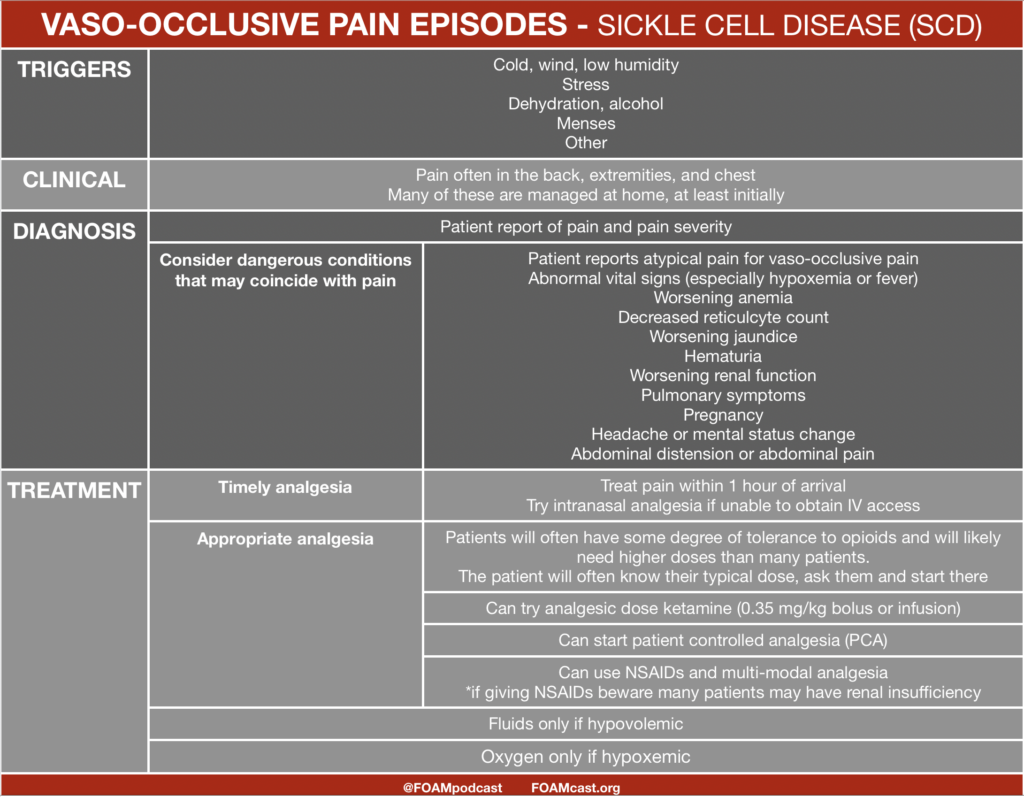
Splenic Sequestration – Second most common cause of death in kids with Sickle Cell Disease <5 years of age.
Classic presentation – LLL: LUQ, lethargy, lightness (pallor).
Labs: 3 point drop in hemoglobin, increased reticulocyte count, and thrombocytopenia.
Generously Donated Rosh Review Questions (Scroll for Answers)
Question 1. [polldaddy poll=8376275]
Question 2. A 23-year-old man presents with a stab wound to the abdomen. His vital signs are HR 132, BP 88/45. He has a positive FAST.[polldaddy poll=8376283]
References:
Chapter 46, 134. Rosen’s Emergency Medicine, 8e.
Chapter 260. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 7e. New York, NY: McGraw-Hill; 2011
Answers.
1. C. Splenic artery aneurysms are the most common type of visceral arterial aneurysms, accounting for up to 60% of cases. Etiologies include arterial fibrodysplasia, portal hypertension, and increased splenic AV shunting in pregnancy. Clinical presentation is vague with left upper quadrant pain with radiation to the left shoulder or subscapular area. Most of the aneurysms are <2 cm in diameter; only 2% result in life-threatening rupture. Treatment is surgical resection if the patient is symptomatic. Otherwise, asymptomatic patients can undergo transcatheter embolization. Of those aneurysms that rupture, up to 95% occur in young pregnant women.
Hepatic artery aneurysms (A) represents 20% of visceral artery aneurysms and are caused by atherosclerosis, infection, and abdominal trauma. Clinical presentation can mimic cholecystitis. Inferior mesenteric artery aneurysms(B) are uncommon. Superior mesenteric artery aneurysms (D) are the 3rd-most common visceral aneurysms. IV drug abusers are at increased risk.
2. D. This patient presents with hemorrhagic shock from a penetrating abdominal trauma and should be immediately transferred to the operating room for an exploratory laparotomy. Stab wounds are the most common form of penetrating trauma. About 70% of anterior stab wounds penetrate the peritoneum. It is difficult to predict the specific organ injured based on the external location of the wound. Initial management should focus on securing the airway, assessing and supporting the patients breathing and circulation. IV access and supplemental oxygen should be provided. In hypotensive trauma patients, early blood transfusion should be initiated and consideration should be made for massive transfusion protocol. Concomitant with the primary and secondary survey, a Focused Assessment with Sonography for Trauma (FAST) exam should be performed. The speed and accuracy of the FAST has almost completely replaced the need for diagnostic peritoneal lavage. In a FAST exam, images are obtained of the splenorenal space, hepatorenal space (Morrison’s pouch), heart and bladder (pouch of Douglas). A FAST exam has high sensitivity in detecting as little as 100 ml of fluid. A FAST examination showing free fluid in any of the abdominal views in the presence of hypotension should lead to the patient being transported to the operating room for exploratory laparotomy according to the Advanced Trauma Life Support (ATLS) algorithm. Angiographic embolization (A) is useful in patients with pelvic fractures and bleeding from pelvic vessels. CT scan of the abdomen and pelvis (B) can be performed in trauma patients who are stable to further assess for injuries.Diagnostic peritoneal lavage (C) does not play a role in management of penetrating trauma patients with hypotension and positive FAST examination.