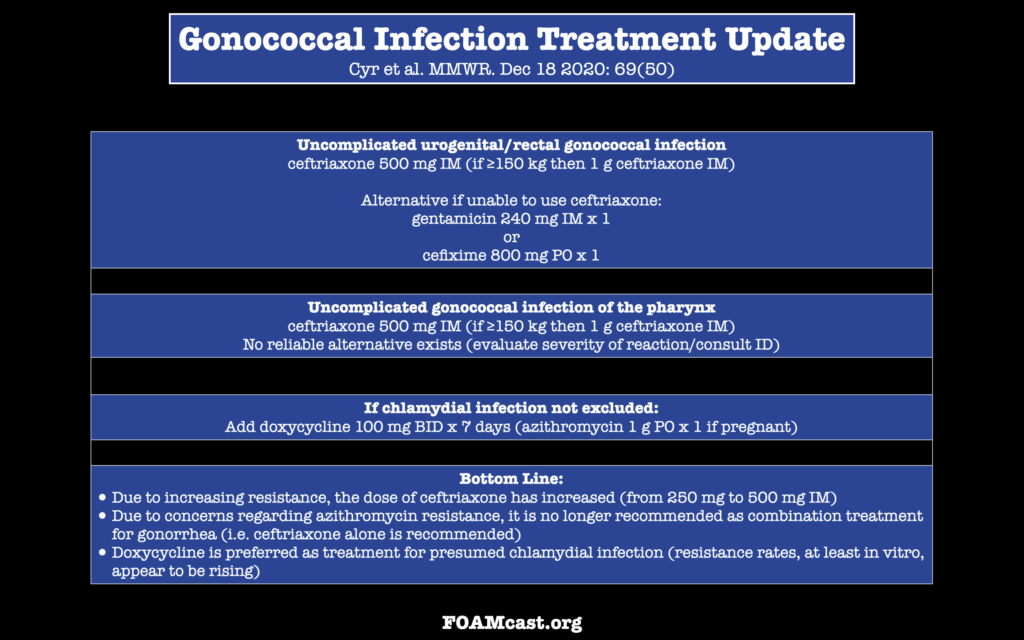
In December 2020, the CDC released updated treatment recommendations for gonococcal infections.
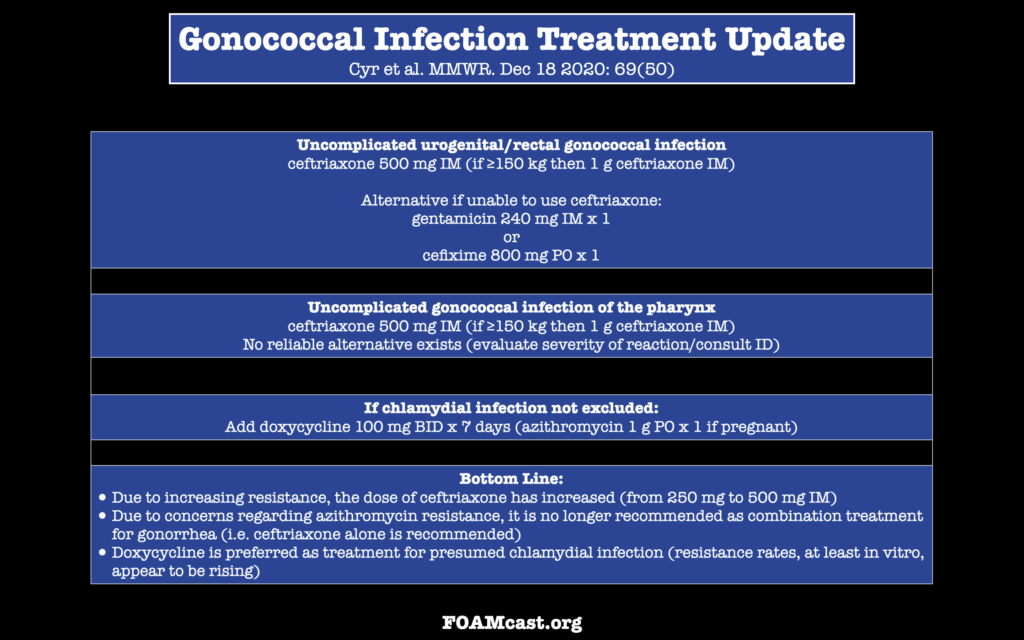
In December 2020, the CDC released updated treatment recommendations for gonococcal infections.
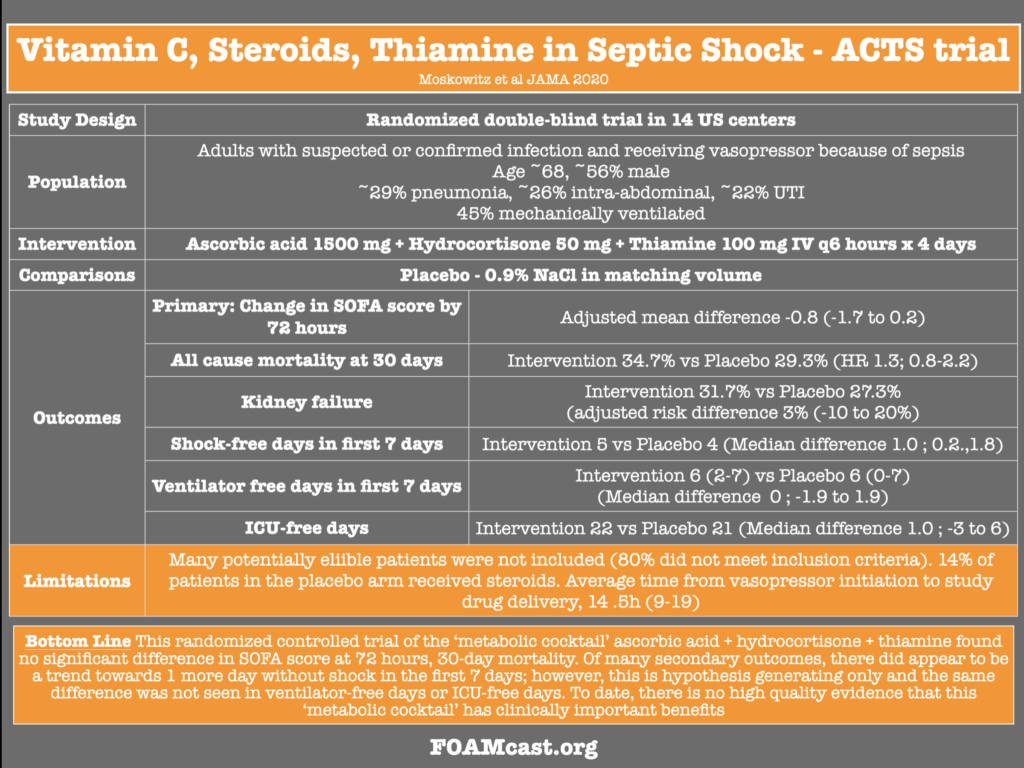
Previously, we have discussed metabolic resuscitation in septic shock (VITAMINS trial) We review the Ascorbic Acid, Corticosteroids, and Thiamine in Septic Shock (ACTS) Trial by Moskowitz et al in JAMA
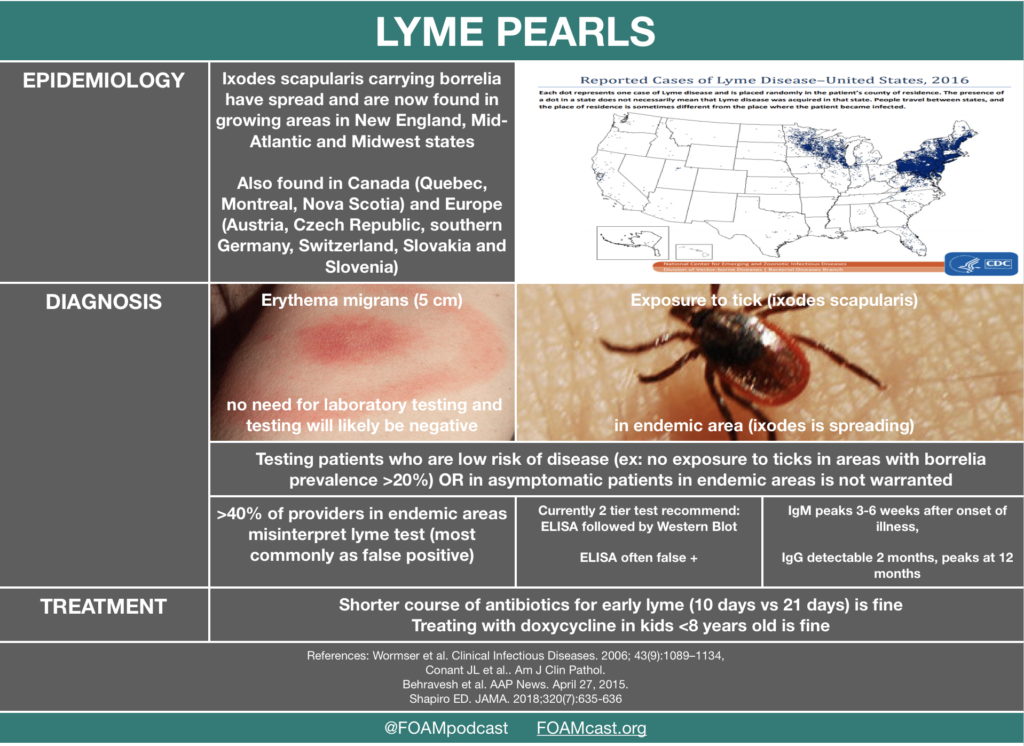
We cover a JAMA Clinical Reviews podcast on lyme disease, including some myth-busters.
Rosh Review Emergency Board Review Questions
A 32-year-old man with a history of hypertension and sickle cell disease presents to the ED for intermittent fevers. He has been feeling ill for the past few weeks with intermittent headaches, night sweats, and abdominal pain. He recently returned from Maine after a trip to see the fall colors. His vital signs are only remarkable for a temperature of 100.7oF. Physical exam reveals mild scleral icterus and hepatomegaly. The patient’s Wright stain shows intraerythrocytic rings. What co-infection is common in this disease?
A. Babesia microti
B. Borrelia burgdorferi
C. Francisella tularensis
D. Rickettsia rickettsii
[accordion]
[toggle title=”Answer” state=”closed”]
A.This patient’s presentation is consistent with acute babesiosis infection. Patients are commonly co-infected with Borrelia burgdorferi (Lyme disease) or ehrlichiosis. Risk factors include functional or surgical asplenia, immunocompromised state, and advanced age. This patient likely has functional asplenia given his age and history of sickle cell disease. Diagnosis is confirmed with a Wright or Giemsa stain showing intraerythrocytic rings, similar to malaria. Babesiosis is due to Babesia parasite and transmitted via the Ixodes deer tick. Patients present with a wide array of symptoms from a vague viral syndrome-type symptoms and spiking fevers to hepatomegaly and hemolytic anemia. Patients with risk factors tend to have more severe features including severe hemolysis, jaundice, renal failure, and acute respiratory distress syndrome. Treatment is with atovaquone and clindamycin or azithromycin.
[/toggle]
[/accordion
Which of the following would be the best antibiotic choice for first-line treatment of a 5-year-old who presents to your office with multiple erythema migrans lesions but no cardiac or neurological symptoms?
A. Amoxicillin PO for 14 to 21 days
B. Azithromycin PO for 14 to 21 days
C. Doxycycline PO for 10 to 21 days
D. Ceftriaxone IM for 14 days
[accordion]
[toggle title=”Answer” state=”closed”]
***This is an example of the difference between practice and board exams, which tend to lag behind current knowledge.
Correct-Answer: Amoxicillin PO for 14 to 21 days. Lyme disease is a tick-borne illness that is caused by Borrelia burgdorferi, making it a spirochetal infection. When deciding the medical therapy for Lyme disease, staging is important. Early localized disease usually presents with a “bullseye rash,” otherwise known as erythema migrans. Patients in this stage of disease may have a few constitutional symptoms, such as fever, fatigue, headache, and myalgias. Early disseminated disease is present if patients have multiple erythema migrans, cardiac or neurologic findings. Late disease usually involves persistent arthritis of a large joint or more severe neurological findings such as encephalopathy or polyneuropathy. In the case above, amoxicillin is the best choice of treatment because the patient is under 8 years of age, and, while multiple lesions are present, the patient does not have neurological or cardiac involvement and should be treated with the same therapy as if he had a single lesion. Recommended duration of therapy is between 14 and 21 days. The goal of therapy is to reduce the risk of developing late Lyme disease and to shorten the duration of symptoms. Azithromycin PO for 14 to 21 days (B) is not recommended as a first-line treatment for Lyme disease because it is less effective than amoxicillin. There has been documented resistance to macrolides by some strains of Borrelia burgdorferi. Doxycycline PO for 10 to 21 days (C) is not recommended in this case because of the patient’s age. Tetracyclines are not recommended for children under 8 years of age because they can lead to permanent staining of their teeth. Ceftriaxone IM for 14 days (D) is not recommended because oral antibiotics, such as doxycycline, are just as effective for treatment of erythema migrans and make for easier administration.
[/toggle]
[/accordion
References:
We tackle some free open access medical education from the CDC on the flu vaccine, including:
Oseltamivir for Influenza
We review the CDC recommendations as well as evidence from a 2014 Cochrane Review [1,3]. The data from the most recent Cochrane review includes studies from Roche Pharmaceuticals (makers of oseltamivir) that were initially unpublished and only released with international pressure, and seemingly do not support the CDC recommendations.
Rosh Review Emergency Board Review Questions
A 74-year-old woman presents with complaints of fever, productive cough with bloody sputum, shortness of breath, and headache. These symptoms developed and worsened drastically over the past 3 days. She recently recovered from an influenza infection 1 week ago. Her medical history otherwise includes only well-controlled hypertension. Vital signs on presentation are as follows: T 39°F, HR 106, BP 110/75, RR 30, oxygen sat 95% RA. A chest radiograph is obtained and a subsequent CT scan of the chest demonstrates multiple cavitary lung lesions. Which of the following organisms is most likely responsible for this patient’s presentation?
A. Clostridum perfringens
B. Escherichia coli
C. Mycobacterium tuberculosis
D. Staphylococcus aureus
[accordion]
[toggle title=”Answer” state=”closed”]
Clostridial gas gangrene is a highly lethal necrotizing soft tissue infection of skeletal muscle caused by toxin- and gas-producing Clostridium species. Clostridium perfringens (A), previously known as Clostridium welchii, is the most common cause of clostridial gas gangrene (80-90% of cases). Escherichia coli (B) is one of the most frequent causes of many common bacterial infections, including cholecystitis, bacteremia, cholangitis, urinary tract infection (UTI), and traveler’s diarrhea, and other clinical infections such as neonatal meningitis and pneumonia. Mycobacterium tuberculosis (C) causes cavitary lung lesions in the upper lobes and clinically manifests as hemoptysis, weight loss and night sweats. It does not have any clinical correlation with influenza.
[/toggle]
[/accordion]
References
We cover Free Open Access Medical Education (FOAM) from a recent Emergency Medicine Cases podcast and First10inEM blog post by Dr. Justin Morganstern regarding urinary tract infections (UTIs). This podcast and blog tackle common issues in UTI diagnosis and treatment, including the following points:
The Core Content
Rosen’s Emergency Medicine (8th ed), Chapter 99; Tintialli’s Emergency Medicine (8th ed), Chapter 91; IDSA Guidelines for Treatment and Asymptomatic Bacteriuria
Rosh Review Emergency Board Review Questions
A 6-year-old girl presents with 4 days of lower abdominal pain. The patient complains of dysuria. On exam, the patient is afebrile and has mild tenderness to palpation in the suprapubic area. No costovertebral tenderness is elicited on exam. A clean-catch urine sample is sent for urinalysis. If positive, which of the following is the most specific to confirm the diagnosis?
A. Glucose
B. Leukocyte esterase
C. Nitrites
D. WBCs (>5 per high power field)
[accordion]
[toggle title=”Answer” state=”closed”]
C. The patient’s presentation is consistent with an uncomplicated urinary tract infection (UTI). The most common cause of a UTI in children >1 year of age is E. coli. Nitrites normally are not found in urine but result when bacteria reduce urinary nitrates to nitrites. Many Gram-negative and some Gram-positive organisms are capable of this conversion, and a positive dipstick nitrite test indicates that these organisms are present in significant numbers (i.e., more than 10,000 per mL). This test is specific (92%–100%) but not highly sensitive (19%–48%). A positive result is helpful, but a negative result does not rule out UTI. The nitrite dipstick reagent is sensitive to air exposure, so containers should be closed immediately after removing a strip. After 1 week of exposure, 33% of strips give false-positive results, and after 2 weeks, 75% give false-positive results. Non-nitrate-reducing organisms also may cause false-negative results, and patients who consume a low-nitrate diet may have false-negative results.

Glucose (A) normally is filtered by the glomerulus, but it is almost completely reabsorbed in the proximal tubule. Glycosuria occurs when the filtered load of glucose exceeds the ability of the tubule to reabsorb it (i.e., 180–200 mg per dL). Etiologies include diabetes mellitus, Cushing’s syndrome, liver and pancreatic disease, and Fanconi’s syndrome. Leukocyte esterase (B) is produced by neutrophils and may signal pyuria associated with UTI. It has a sensitivity of 72%–97% and specificity of 41%–86%. Leukocyte casts in the urinary sediment can help localize the area of inflammation to the kidney. Organisms such as Chlamydia and Ureaplasma urealyticum should be considered in patients with pyuria and negative cultures. Other causes of sterile pyuria include balanitis, urethritis, tuberculosis, bladder tumors, viral infections, nephrolithiasis, foreign bodies, exercise, glomerulonephritis, and corticosteroid and cyclophosphamide use. Leukocytes (D) may be seen under low- and high-power magnification. Men normally have fewer than 2 white blood cells (WBCs) per HPF; women normally have fewer than 5 WBCs per HPF; >5 WBCs/HPF is associated with a 90%–96% sensitivity and 47%–50% specificity.
[/toggle]
[/accordion]
A 24-year old woman presents with URI symptoms. She is 32 weeks pregnant. As part of her work-up, you order a urinalysis, which shows 2+ bacteria with no WBCs. Two days later, the lab calls you and informs you that the urine culture is positive. You call the patient back and she denies symptoms of urinary tract infection. With regards to the urine culture results, what treatment is indicated?
A. Cephalexin 500 mg QID for 7 days
B. Ciprofloxacin 500 mg QID for 7 days
C. No treatment is necessary
D. Trimethoprim-sulfamethoxazole 1 DS tablet BID for 3 days
[accordion]
[toggle title=”Answer” state=”closed”]
A. The patient has asymptomatic bacteriuria of pregnancy confirmed by a positive urine culture and should be treated with an oral antibiotic that is known to be safe in pregnancy, such as cephalexin 500 mg QID for 7 days. Asymptomatic bacteriuria is common in the general population and in most scenarios does not require therapy. However due to the high risk of complication seen during pregnancy, it should be treated with antibiotics. It is seen in 2-10% of pregnant women and is commonly due to E. coli. Pregnant women have an increased risk of developing urinary tract infections due to the pressure that the enlarged uterus exerts on the ureters and bladder, incomplete emptying during voiding and impaired ureteral peristalsis from progesterone-induced relaxation of the ureteral smooth muscle. Complications of untreated asymptomatic bacteriuria include development of a lower urinary tract infection, pyelonephritis, renal abscess, renal failure, bacteremia, sepsis, intrauterine growth retardation, premature labor and neonatal death. Treatment options generally include cephalosporins, such as cephalexin, amoxicillin (or amoxicillin-clavulanate) and nitrofurantoin. All of which are recognized as Category B by the Food and Drug Administration; meaning that animal studies have failed to show a risk to the fetus. Treatment duration should be for 7-10 days.

Ciprofloxacin (B) and trimethoprim-sulfamethoxazole (D) are Category C and D, respectively, and therefore should be avoided in pregnancy when possible. Because there is increased risk for complication during pregnancy, antibiotic treatment (C) is recommended.
[/toggle]
[/accordion]
References:
Gupta K et al. International Clinical Practice Guidelines for the Treatment of Acute Uncomplicated Cystitis and Pyelonephritis in Women: A 2010 Update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Infect Dis (2011) 52 (5): e103-e120.
Nicolle L et al. Infectious Diseases Society of America Guidelines for the Diagnosis and Treatment of Asymptomatic Bacteriuria in Adults. Infect Dis (2005) 40 (5): 643-654.
Rosen’s Emergency Medicine, 8th ed. Chapter 99.
Tintinalli’s Emergency Medicine, 8th ed. Chapter 91.
We cover an episode of The Skeptic’s Guide to Emergency Medicine that covers a validation study of the Step by Step approach to pediatric fever. This approach to infants with a fever <3 months old is alluring as it does not necessitate a lumbar puncture. This algorithm had a better sensitivity and negative predictive value than the Rochester criteria. The approach did miss some infants with a serious bacterial infection and these tended to be those between 21 and 28 days old and those with fever onset <2 hours prior to arrival.
Core Content
We cover Chapter 116 in Tintinalli’s Emergency Medicine (8th ed) and Rosen’s on pediatric fever.
Infants <3 months old with fever algorithms
Rosh Review Emergency Board Review Questions
A 25-day-old female presents with fever and cough. Mom denies any symptoms at home. The patient’s 2-year-old brother had a cough and rhinorrhea 1 week prior. On exam, the patient’s temperature is 38.7°C with clear lungs, a benign abdomen, and normal tympanic membranes bilaterally. What is the appropriate workup for this patient?
[accordion]
[toggle title=”Answer” state=”closed”]
4. Neonates with fever aged 28 days or younger may have few clues on history and physical examination to guide therapy. Therefore, a high index of suspicion is necessary to detect the febrile neonate with a serious bacterial infection. Obtaining the pertinent medical history from the mother regarding the pregnancy, delivery, and early neonatal life of the febrile neonate is essential. Typically, infections in the 1st week of life are secondary to vertical transmission, and those infections after the 1st week are usually community acquired or hospital acquired. Bacterial meningitis is more common in the 1st month of life than at any other time. An estimated 5%–10% of neonates with early onset group B streptococcal (GBS) sepsis have concurrent meningitis. Therefore, febrile infants (temperature >38°C) younger than 28 days should receive a full sepsis workup. CBC, chest X-ray (A), urinalysis (B), and blood cultures (C) are a partial workup for neonatal fever.
[/toggle]
[/accordion]
A two-day-old boy presents to the ED with fever for the past four hours. His birth history includes a normal spontaneous vaginal delivery at term. Parents report noticing that the child “felt warm,” and that he was having copious nasal secretions while feeding. On physical examination, the child appears lethargic, has mottled extremities, and is hot to the touch. Breath sounds are clear bilaterally, and there are no rashes. His vital signs are T 102.9°F, BP 74/48 mm Hg, HR 170 beats per minute, and RR 40 breaths per minute. Which of the following groupings of organisms should your antibiotic choices cover when treating this febrile neonate?
Answer 1. The febrile neonate is a child 28 days and younger who presents with a fever. These children are at very high risk of serious bacterial infections, including urinary tract infection, pneumonia, meningitis, and bacteremia. Risk factors for serious bacterial infection in a neonate include prematurity, low birth weight, premature or prolonged rupture of membranes, meconium aspiration, or maternal group B streptococcus infection. The evaluation of a neonate with a fever includes CBC, urinalysis, blood culture, urine culture, and a lumbar puncture in order to obtain CSF for cell count, Gram stain, and culture. If the child has respiratory symptoms, a chest X-ray should be performed. If the child has diarrhea, stool testing should also be performed. The most common pathogens involved in serious bacterial infections, including meningitis and bacteremia, in neonates are Listeria monocytogenes, Group B streptococcus, and Escherichia coli. These children can become critically ill very rapidly; therefore, initial management should include a fluid bolus of 20 mL/kg and broad-spectrum antibiotics to cover the most common pathogens in this age group. The most appropriate antibiotics to use in neonates with a fever are ampicillin and cefotaxime. Ampicillin will cover Listeria monocytogenes while cefotaxime will cover Group B streptococcus and Escherichia coli. If there is a history of maternal infection with herpes simplex virus, acyclovir should be added to the empiric broad-spectrum treatment. These patients universally need to be admitted to the hospital for IV antibiotics and observation until all cultures have returned. Mycoplasma pneumoniae, Neisseria meningitidis, Streptococcus pneumoniae (B) are common pathogens seen in adolescents and young adults. Mycoplasma pneumoniae is a common cause of atypical pneumonia in this age group. Streptococcus pneumoniae is a common bacterial cause of pneumonia, bacteremia, and meningitis while Neisseria meningitidis is primarily a cause of meningitis. Neisseria meningitidis, Listeria monocytogenes, Streptococcus pneumoniae (C) are the primary pathogens causing serious bacterial infections in adults over the age of 65. Listeria monocytogenes is a pathogen that is seen in infants and then later reemerges as a prominent pathogen in older adults. Streptococcus pneumoniae, Neisseria meningitidis, Haemophilus influenzae (D) are the most common pathogens causing serious bacterial infections in children ages one to five years. There has been a significant decline in the incidence of Haemophilus influenzae type B in recent years due to childhood vaccination programs.
[/toggle]
[/accordion]
Core Content
We delve into core content on red flags in back pain and spinal epidural abscess using Rosen’s Emergency Medicine and Tintinalli’s Emergency Medicine Chapter 279 as a guide.
Rosh Review Emergency Board Review Questions
A. An appropriate antibiotic regimen is cefepime and metronidazole
B. Direct extension of skin and soft tissue infections is the most common cause
C. Erythrocyte sedimentation rate is a sensitive screening tool
D. Most patients present with back pain, fever, and a focal neurologic deficit
[accordion]
[toggle title=”Answer” state=”closed”]
C. Erythrocyte sedimentation rate is a sensitive screening toolThe patient has a posterior epidural abscess with adjacent osteomyelitis and myositis. The most common cause of an epidural abscess is hematogenous spread of infection, not direct extension from skin or soft tissue infection. Major risk factors include diabetes, intravenous drug abuse, chronic renal failure, alcoholism, and immunosuppression. The most common organism involved is Staphylococcus aureus. Other organisms include streptococci, anaerobes, gram-negative bacilli, and Pseudomonas aeruginosa. Patients present with localized back pain with tenderness to percussion. Fevers are common (reported in up to 75% of patients). MRI is the diagnostic modality of choice, but erythrocyte sedimentation rate is a sensitive marker and may be used in conjunction with plain radiographs to screen for infectious spinal disease.Vancomycin is an important component of the antibiotic regimen because it covers methicillin-resistant Staphylococcus aureus (MRSA) and is usually combined with a 3rd-generation cephalosporin (A). Cefepime is a 4th-generation cephalosporin with pseudomonas coverage. Metronidazole or clindamycin can be added for anaerobic coverage. While the classic triad consists of back pain, fever, and neurologic deficits (D), only a small proportion of patients actually have all three components at presentation. The most common cause of an epidural abscess is hematogenous spread of infection, not direct extension from skin or soft tissue infection (B).
[/toggle]
[/accordion]
An 8-year-old previously healthy boy presents with back pain and fever for 4 days. He complains of pain in the low back, which is increased with bending or twisting. The pain radiates down into his left leg. He denies trauma. Physical exam is remarkable only for tenderness to palpation over the lumbar spine. What management is indicated
A. Ibuprofen and follow up with his pediatrician
B. MRI of the lumbar spine
C. Plain radiographs of the lumbar spine
D. Urinalysis
[accordion]
[toggle title=”Answer” state=”closed”]
B.
MRI of the lumbar spine. This patient presents with symptoms consistent with discitis and should have an MRI for diagnosis. Discitis is a rare infection of the nucleus pulposus and can involve the cartilaginous endplate and vertebral body. It can occur spontaneously or after surgical procedures. Typically, patients present with severe pain localized to the spinal level of involvement. Any movement of the spine exacerbates the pain. Children often present with sudden onset of back pain and refusal to walk. The lumbar spine is most commonly involved and the average age of patients is 7 years. Radicular symptoms are common (present in 50-90% of cases) and most patients will present with fever (90%). Neurologic deficits are uncommon. Serious pathology should be suspected in any pediatric patient presenting with back pain. Neurologic symptoms are rarely present. MRI is the best study for diagnosis and can also rule out other critical diagnoses including epidural abscess. Laboratory studies are non-specific and insensitive but typically will have an elevated erythrocyte sedimentation rate. White blood cell counts are frequently within the normal range.
[/toggle]
[/accordion]
Ultrasound is gaining popularity in assisting lumbar punctures (LPs). We review this technique as well as Free Open Access Medical Education (FOAM) from the following sites: 5 Min Sono, Sinai EM, and PEM pearls from ALiEM.
We then delve into core content on meningitis, encephalitis, and antiNMDA receptor encephalitis using Rosen’s Chapter 109 and Tintinalli’s Chapters 117 and 174 as a guide.
Rosh Review Emergency Board Review Questions
A 40-year-old man with HIV presents with two weeks of progressive headache, malaise, and fever. On examination, he has mild nuchal rigidity, confusion, and a temperature of 38.2oC. Cerebrospinal fluid analysis shows a white blood cell count 360 cells/mL with a monocyte predominance, glucose 28 mg/dL, and protein 220 mg/dL. What is the treatment of choice?
A. Acyclovir
B. Amphotericin B
C. Ceftriaxone
D. Vancomycin
[accordion]
[toggle title=”Answer” state=”closed”]
B. Amphotericin B . Cryptococcal meningoencephalitis is an opportunistic infection that occurs primarily in patients with advanced AIDS, although it can be seen in immunocompromised transplant patients as well. The majority of HIV-related cases occur when the CD4 count is < 100 cells/mm3. Patients present with progressive headache, nausea, malaise, and fever over the course of 1 – 2 weeks. Examination findings are typical for meningitis and include altered mental status, photophobia, and fever. Meningismus is less commonly seen. Presentations can be subtle and a high index of suspicion is needed for diagnosis. A CT scan of the brain is indicated if there are signs of increased intracranial pressure or focal neurologic deficits. Lumbar puncture should be performed with careful measurement of the opening pressure. Cerebrospinal fluid will show a mildly elevated white blood cell count with a monocyte predominance, decreased glucose, and mildly elevated protein. However, in some cases the cerebrospinal fluid will only show minor, if any, abnormalities. Cryptococcal antigen testing of the CSF is nearly 100% sensitive and specific. India ink staining will show budding organisms. Treatment of choice is intravenous amphotericin B in addition to oral flucytosine for 14 days followed by an 8 week course of oral fluconazole. Acyclovir (A) is used in the treatment of herpes meningoencephalitis. Ceftriaxone (C) and vancomycin (D) are indicated in the treatment of bacterial meningitis.
[/toggle]
[/accordion]
A previously healthy 18-year-old woman presents to the emergency department with complaints of fever, headache, and neck stiffness. She is accompanied by her sister, who expresses concern because the patient seems suddenly confused and cannot remember what she did yesterday. After you administer empiric intravenous antibiotics, which of the following is the next best step?
A. Chest X-ray
B. Complete blood count with differential
C. Lumbar puncture
D. Urinalysis
[accordion]
[toggle title=”Answer” state=”closed”] C. Lumbar puncture. Meningitis is an inflammation of the tissues surrounding the brain and spinal cord (meninges) and may be of infectious (bacterial, viral, or fungal) and various other etiologies. The classic clinical manifestations include nuchal rigidity, fever and altered mental status. Patients often present with headache as well. All patients with suspected meningitis should have lumbar puncture (LP) to evaluate the cerebrospinal fluid (CSF) unless this procedure is contraindicated. There are no absolute contraindications to LP. Relative contraindications include patients with evidence of increased intracranial pressure, thrombocytopenia, bleeding diathesis or spinal epidural abscess. Acute bacterial meningitis is a medical emergency and left untreated or treated late is almost universally fatal. Treatment involves addressing systemic complications and initiating empiric antibiotic therapy as soon as possible.
Up to half of patients with pneumococcal meningitis may have evidence of pneumonia on chest X-ray (A), but this is not part of the initial workup of patients with suspected meningitis. Complete blood count with differential (B) is often ordered in the workup for bacterial meningitis and generally shows increased white blood cell count, but is not as important to order initially as an LP. Urinalysis (D) is generally not a helpful test in the diagnosis of meningitis and therefore not recommended in the workup for patients with suspected bacterial meningitis.
[/toggle]
[/accordion]
References:
(ITUNES OR LISTEN HERE)
The Free Open Access Medical Education (FOAM)
Life in the Fast Lane Research and Reviews (LITFL R&R) #121 featured a section on the new American Gastroenterology Association (AGA) guidelines on diverticulitis. The game changer? Antibiotics aren’t a requirement in select patients with uncomplicated acute diverticulitis [1].
The guidelines based this recommendation on two studies, previously covered by Dr. Ryan Radecki on Emergency Medicine literature of note over the past 3 years. This post details a prospective observational study on antibiotics for acute diverticulitis [2]. In another post, Dr. Radecki discusses an RCT of antibiotics (ABX) vs IV fluids only.
Of note, since 2012, the Cochrane Review suggests that antibiotics may not be necessary in uncomplicated appendicitis [4].
A note on LITFL R&R – every week this blog post features 5-10 high yield articles, culled from contributors across the globe from all kinds of literature – pediatrics, critical care, emergency medicine, etc. It is difficult to keep up with the literature and some have estimated that the number needed to read (NNR) to of 20-200, depending on the journal [5]. Those looking for high yield articles may find their time well spent focused on this cherry picked selection of articles.
Core Content
We delve into core content on diverticula and clostridium difficile using Rosen’s Medicine (8e), Chapters 31, 173 and Tintinalli’s Emergency Medicine: A Comprehensive Study Guide (7e) Chapters 76, 85.
Diverticulosis
Diverticula are small herniations through the wall of the colon (small outpouchings). Often this is asymptomatic, identified incidentally on imaging or colonoscopy. Most common cause of lower gastrointestinal bleeding (LGIB) in adults in the U.S.
Diverticulitis
Clostridium Difficile (c. diff)
Note on testing – asymptomatic carriage rates of c.diff vary based on the population but may be between 3-50%. Textbooks quote a 3% carriage rate in newborns and rates of 20%-50% in hospitals and long term care facilities, respectively [10,11].
C. diff historically has a unique odor, refrains of “it smells like c. diff” echo in the halls. Yet this does not perform very well, essentially a coin flip based on a 2013 study by Rao and colleagues. They had 18 nurses smell 10 stool samples (5 c. diff positive and 5 c. diff neg) and found the median percent correct identification of c. diff positive vs negative was 45% [6].
Rosh Review Questions
Question 1. [polldaddy poll=9330955]
Question 2.A 75-year-old woman presents with several days of voluminous watery stools. She was discharged from the hospital one week ago following treatment for pneumonia. Stool studies reveal C. difficile toxin. [polldaddy poll=9333580]
Answers:
References:
(ITUNES OR LISTEN HERE)
The Society of Critical Care Medicine (SCCM) and the European Society of Intensive Care Medicine (ESICM) redefined sepsis with the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). Sepsis is life-threatening organ dysfunction due to dysregulated host responses to infection. Septic shock is a subset of sepsis where underlying circulatory and cellular/metabolic abnormalities are profound enough to substantially increase mortality [2].
2003 vs 2016 Definitions of Sepsis [1-4]
Systemic Inflammatory Response Syndrome (SIRS) is out.
qSOFA is in. a qSOFA score of 2 or 3 or a rise in the SOFA score of 2. The SOFA score requires a ton of lab values so the authors wanted something that could be assessed at triage, hence the quick SOFA score (qSOFA). The authors derived and retrospectively validated this score and compared it to SIRS in a cohort of 148,907 patients [3]
Issues:
Notes: Sepsis rates have increased over the past 10 years and it appears that mortality has decreased. However, less sick patients are included in this. It appears that the Sepsis 3 authors were hoping for a more specific definition.
References: