The Free Open Access Medical Education (FOAM)
We cover an incredible ophthalmology resource, OphthoBook.com, by Dr. Tim Roots. This resource has a free book and excellent free video lectures. Specifically, we detail a hilarious video on eye exam tricks, especially targeting individuals who “can’t see.”
[table id=3 /]
- Core Content
- We previously reviewed eye trauma in this podcast. In this episode, we review ophthalmology basics using Tiintinalli’s Emergency Medicine Chapter 241.
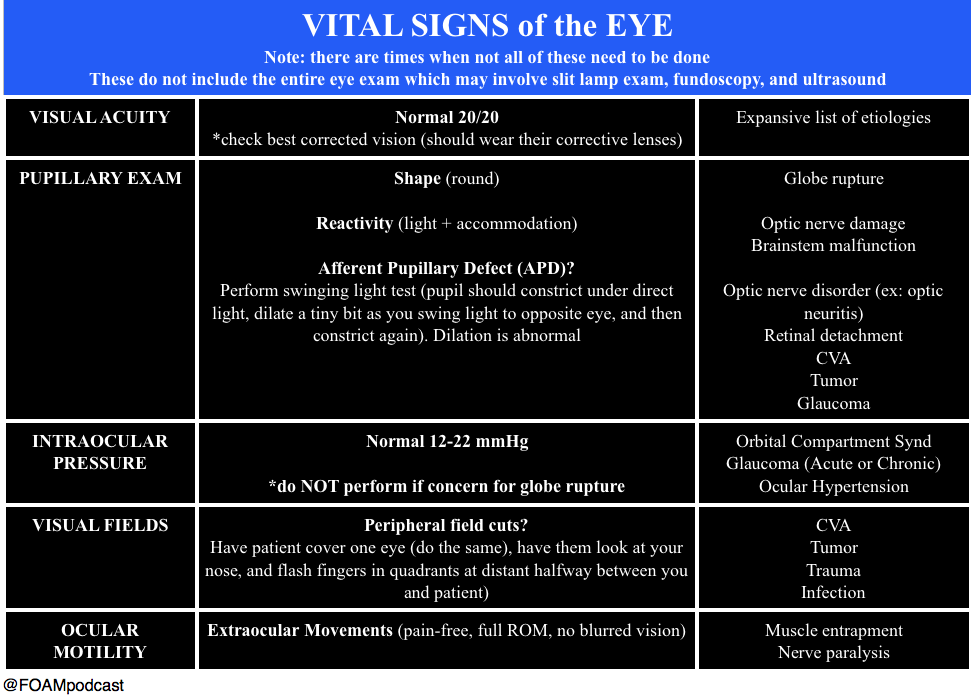
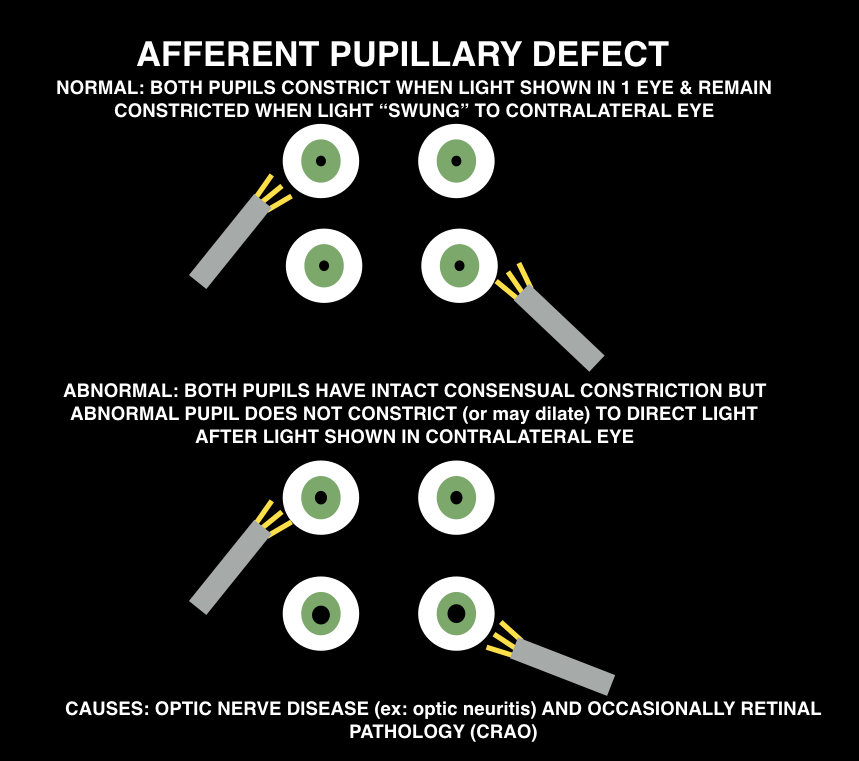
When doing the pupillary exam, it is important to assess for an afferent pupillary defect (APD). Ophthalmologists will want “there is or is NOT an APD” when you consult them for essentially any reason. Normal pupils constrict when the light is shown in either pupil (direct and consensual constriction). To assess for an APD, perform the “swinging light test.”
Causes: optic nerve pathology (ex: optic neuritis) or occsaionally, retinal pathology (CRAO)
Peer reviewed by Michael Westafer, MD ophthalmologist and glaucoma fellow at Cleveland Clinic.
Generously Donated Rosh Review Questions
A 72-year-old man presents with a painful red eye and visual loss worsening over the last 24 hours. He recently had cataract surgery. Examination of the eye reveals the image above. Which of the following is the most likely?
A. Endophthalmitis
B. Hyphema
C. Uveitis
D. Vitreous hemorrhage
[accordion]
[toggle title=”Answer” state=”closed”]
A. Endophthalmitis is an infection involving the anterior, posterior and vitreous chambers of the eye. It results from trauma (blunt globe rupture, penetrating injury, foreign bodies) and alsoiatrogenically after ocular surgery like cataract repair. Patients complain of severe pain in the eye and visual impairment or loss. Examination of the eye reveals decreased visual acuity, injected conjunctiva, chemosis and haziness of the infected chambers. Infections are treated with both systemic and intraocular antibiotics.
A hyphema (B) is blood in the anterior chamber usually caused by trauma. When the patient is in an upright position, blood will layer along the inferior aspect of the anterior chamber. As the hyphema increases in size, it elevates intraocular pressure. In some cases admission is warranted for patients with large hyphemas (>50%), decreased vision, sickle cell disease and elevated intraocular pressure. Treatment is aimed at decreasing pressure with topical (beta-blocker, alpha agonist or carbonic anhydrase inhibitors) and systemic therapy (carbonic anhydrase inhibitor, mannitol). Uveitis (C) occurs after blunt trauma in which the iris and ciliary body are inflamed causing ciliary spasm. Patients complain of significant photophobia with significant eye pain. Examination of the eye reveals perilimbal conjunctival injection (also called ciliary flush) and a small, poorly dilating pupil. Photophobia occurs with light shone on both the affected and unaffected eye. On slit lamp, cells (white and red) and flare (protein) are noted in the anterior chamber. Treatment is with a topical cycloplegic agent to minimize spasm. Vitreous hemorrhage (D) occurs as a result of injuries to the retina, uveal tract and their associated vascular structures. Common associated conditions include diabetic retinopathy, retinal vein occlusion and trauma. Patients complain of decreased visual acuity and floaters. The condition is not typically painful. Diagnosis is made with ocular ultrasound showing blood products in the posterior chamber.
[/toggle]
[/accordion]
What is a dependent pocket of pus seen in the anterior chamber called?
- [accordion]
- [toggle title=”Answer” state=”closed”]
- Hypopyon.
- [/toggle]
- [/accordion]
A 51-year-old man walks into a movie theater and experiences acute onset of right eye pain associated with nausea, vomiting, and cloudy vision. Which of the following is expected during the ophthalmologic exam?
A. Cherry-red spot in the macular area
B. Deep anterior chamber
C. Intraocular pressure >21 mm Hg
D. Miotic pupil
[accordion]
[toggle title=”Answer” state=”closed”]
The patient has acute angle-closure glaucoma. This condition results in optic nerve damage from increased intraocular pressure. In patients with a narrow anterior chamber angle, reduced illumination (like entering a dark movie theater) causes mydriasis. Subsequently, folds of the peripheral iris can block the angle, which prevents aqueous humor outflow. This leads to a rapid elevation of intraocular pressure causing ocular pain, a hazy cornea, ciliary flush, a firm globe, and optic nerve damage if the pressure is not promptly relieved. An intraocular pressure >21 mm Hg is considered elevated. Pressures can elevate quickly to >60 mm Hg. The higher the pressure, the quicker damage occurs to the optic nerve and the poorer the prognosis. The diagnosis is often delayed due to the associated symptoms of nausea, vomiting, and abdominal pain. Treatment involves reducing aqueous humor production with IV acetazolamide, topical beta-blockers (timolol), and topical alpha-agonists (apraclonidine). Topical miotic agents (pilocarpine) are used to reverse the angle closure. Topical steroidshelp to reduce inflammation. Hyperosmotic agents (mannitol, glycerol) can also be administered for further reduction in intraocular pressure.
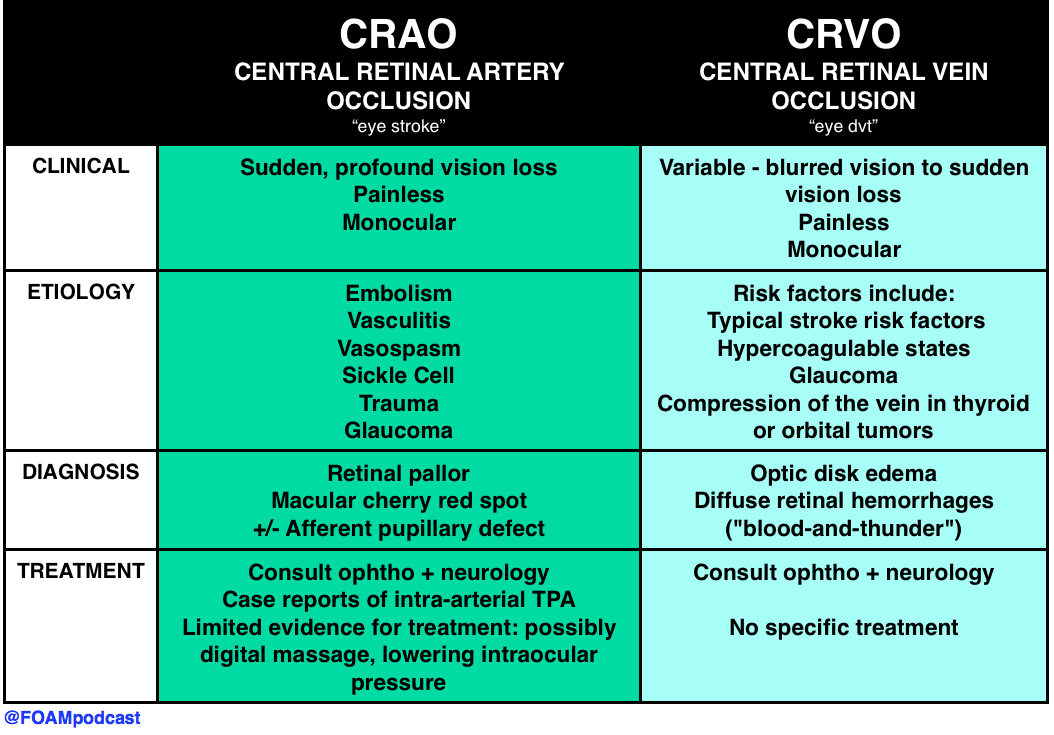
The funduscopic finding of a pale retina with a cherry-red spot in the macular area (A) is consistent with central retinal artery occlusion. This condition is associated with sudden unilateral vision loss that is painless. It is caused by a thrombotic plaque or embolus of the central retinal artery. A deep anterior chamber (B) is protective against acute angle-closure glaucoma. Individuals with a narrow chamber are at increased risk. The pupil in acute angle-closure glaucoma is most commonly fixed and mid-dilated, rather than miotic (D). Miotic pupils are associated with opiate use, cholinergic toxicity, and pontine strokes.
[/toggle]
[/accordion]
References:
“Eye Emergencies.” Chapter 241. Tintinalli’s Emergency Medicine: A Comprehensive Review. 8th ed.