(ITUNES OR Listen Here)
The Free Open Access Medical Education (FOAM)
This week we cover a post from Dr. Rory Spiegel, author of EMnerd, on initial nonoperative management of acute appendicitis based on an article by Salminen et al in JAMA 2015.
- 530 patients with CT confirmed acute, uncomplicated appendicitis were randomized to operative intervention (n=273 receiving open laparotomies) or non-operative intervention (n=257 receiving antibiotics).
- 27.3% (n=70, CI 22-33.2%) of patients who received medical management (ertapenem x 3 days then 5 days of levofloxacin) had an appendectomy by the 1 year mark
- 7 patients (2.7%) in medical management group had complicated appendicitis at one year, 0 had abscesses
- 45 patients (20.5%) in the operative group had surgical complications
This is a non-inferiority study where the intent is to demonstrate that an experimental treatment (antibiotics alone) is not substantially worse than a control treatment (immediate surgery). The authors set the non-inferiority margin at 24%, which means that a failure rate (appendectomy by 1 year) >24% would render medical management inferior.
Authors Conclusion: “Among patients with CT-proven, uncomplicated appendicitis, antibiotic treatment did not meet the prespecified criterion for noninferiority compared with appendectomy.”
Spiegel’s Conclusion: “there is a great deal to be determined before this non-invasive strategy can be considered mainstream practice…in what was once considered an exclusively surgical disease, the majority of patients can effectively be managed conservatively. Despite not meeting their own high standards for non-inferiority, the authors demonstrated that for most patients with acute appendicitis, when treated conservatively with antibiotics we can avoid surgical intervention without complications of delays to definitive care.”
More FOAM on non-operative treatment of appendicitis: The SGEM
Core Content
Tintinalli (7e) Chapters 84, 124; Rosen’s Emergency Medicine (8e) Chapter 93
Appendicitis
Diagnosis:
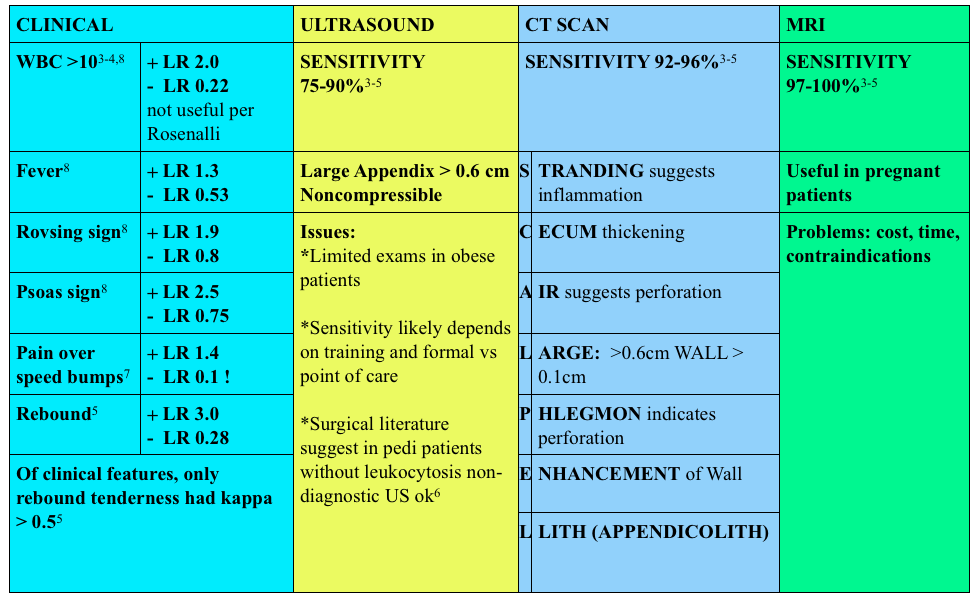
Use of contrast enhanced CT scans controversial. Rosenalli and the American College of radiology concur that oral contrast is probably not needed but does increase the emergency department length of stay [3-5].
Treatment:
- Surgical consult
- Antibiotics:
- Broad spectrum beta-lactams: ampicillin-sulbactam 3g IV (75 mg/kg IV in peds) piperacillin-tazobactam 4.5g IV, cefoxitin 2g IV (40 mg/kg IV in peds) OR metronidazole 500 mg IV + ciprofloxacin 400 mg IV
Other things to consider in special populations in right lower quadrant:
Pelvic Inflammatory Disease and Tubo-Ovarian Abscess in women
- Symptoms: vaginal discharge, adnexal or uterine tenderness, lower abdominal pain, cervical motion tenderness, fever
- Cause: chlamydia and neisseria gonorrhoea most commonly
- Treatment: ceftriaxone 250 mg IM + doxycycline 100 mg BID x 14 days
Typhlitis (neutropenic enterocolitis) –
- Symptoms: crampy abdominal pain (often RLQ), abdominal distension, fever, diarrhea, bloody diarrhea
- Diagnosis: CT scan
- Treatment: NPO, IV fluids, broad spectrum antibiotics (piperacillin-tazobactam, meropenem, metronidazole) + surgical consult if needed
- Complications: perforation, gastrointestinal bleeding, sepsis
Generously Donated Rosh Review Questions
1. A 22-year-old man presents with abdominal pain followed by vomiting for 1 day. His examination is significant for right lower quadrant tenderness to palpation. He has a negative Rovsing sign. [polldaddy poll=9026936]
2. A 22-year-old woman presents with lower abdominal pain and vaginal discharge. She is sexually active with men with inconsistent barrier protection. Her vitals are normal other than temperature of 101°F. On examination, there is yellow cervical discharge, no cervical motion tenderness, but uterine and left adnexal tenderness. An ultrasound does not show any evidence of tubo-ovarian abscess. [polldaddy poll=9026939]
Answers.
1. B. Sensitivity or the true positive rate measures the proportion of actual positives that are correctly identified as such. It is determined by dividing the number of true positives of the test by the number of true positives + false negatives. Tests with a high sensitivity are good for ruling out disease as the test has very few false negatives. A test with high sensitivity is advantageous as a screening tool as it misses very few people with the disease. The onset of pain before vomiting has been found to be as high as 100% sensitive in diagnosing acute appendicitis.Rovsing’s sign (D) (indirect tenderness) describes pain felt in the right lower quadrant upon palpation of the left lower quadrant. This sign signifies the presence of peritoneal irritation and has a sensitivity of 58%. Right lower quadrant pain (C) has a sensitivity of 81% and fever (A) has a sensitivity of 67%.
2.This patient presents with signs and symptoms consistent with pelvic inflammatory disease (PID) and should be treated with ceftriaxone 250 mg IM and 2 weeks of doxycycline. PID is an ascending infection beginning in the cervix and vagina and ascending to the upper genital tract. Neisseria gonorrhoeae and Chlamydia trachomatis are most commonly implicated. It can present with a myriad of symptoms although lower abdominal pain is the most common. Other symptoms include fever, cervical or vaginal discharge and dyspareunia. Pelvic examination reveals cervical motion tenderness (CMT), adnexal tenderness and vaginal or cervical discharge. Inadequately treated PID can lead to tubo-ovarian abscess, chronic dyspareunia and infertility. Due to the variable presentation and serious sequelae, the CDC recommends empiric treatment of all sexually active women who present with pelvic or abdominal pain and have any one of the following: 1) CMT, 2) adnexal tenderness or 3) uterine tenderness. Treatment should cover the most common organisms and typically consists of a third generation cephalosporin (ceftriaxone) and a prolonged course of doxycycline. Patients with systemic manifestations or difficulty tolerating PO should be admitted for management.Ceftriaxone and azithromycin (A) are used in the treatment of cervicitis or urethritis. Clindamycin (C) and metronidazole (D) are used in the treatment of bacterial vaginosis.
References:
1.Salminen P, Paajanen H, Rautio T, et al. Antibiotic Therapy vs Appendectomy for Treatment of Uncomplicated Acute Appendicitis: The APPAC Randomized Clinical Trial. JAMA. 2015;313(23):2340
2. Horst JA, Trehan I, Warner BW et al. Can Children With Uncomplicated Acute Appendicitis Be Treated With Antibiotics Instead of an Appendectomy? Ann Emerg Med. 2015;66:(2)119-22
3.”Acute Appendicitis.” Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th ed. pp 574-581.
4. “Acute Appendicitis” Rosen’s Emergency Medicine. 8th ed. pp. 1225-1232.e2
5. ACR Appropriateness Criteria. American College of Radiology. 2013.
6. Cohen B, Bowling J, Midulla P, et al. The non-diagnostic ultrasound in appendicitis: is a non-visualized appendix the same as a negative study? J Pediatr Surg. 2015;50:(6)923-7
7. Ashdown HF, D’Souza N, Karim D, Stevens RJ, Huang A, Harnden A. Pain over speed bumps in diagnosis of acute appendicitis: diagnostic accuracy study. BMJ. 2012;345:e8012.
8. Bundy DG, Byerley JS, Liles EA. Does This Child Have Appendicitis? 2009;298(4):438–451.
Faust here. I think the WBC count is interesting. As above, it is not so useful for helping in the diagnosis of acute appendicitis BUT, Rosen’s notes that fewer that 4% of PERFORATED appys will have a normal white count. So it might risk stratify some of these patients.
Faust here. I think the WBC count is interesting. As above, it is not so useful for helping in the diagnosis of acute appendicitis BUT, Rosen’s notes that fewer that 4% of PERFORATED appys will have a normal white count. So it might risk stratify some of these patients.