(iTunes or listen here)
The Free Open Access Medical Education (FOAM)
This week we review a post from Academic Life in Emergency Medicine, written by Brent Reed on selecting rate control agents in the management of atrial fibrillation. This is a follow up post to Bryan Hayes’ summary of emergency department (ED) management of acute atrial fibrillation. Both are high yield.
Acute Management:
- No clear cut winner in the beta-blocker vs. calcium channel blocker battle
Long Term Atrial Fibrillation Management in General:
Avoid beta-blockers in:
- Obstructive lung disease (asthma/COPD)
- Peripheral vascular disease
- Diabetics
- Severe congestive heart failure (CHF)
- Erectile dysfunction
Avoid calcium-channel blockers in:
- Severe CHF and acute decompensated heart failure (ADHF)
Of note, in patients
The Maryland Critical Care Project has a great post with many of Dr. Amal Mattu’s key FOAM talks embedded on Tachydysrhythmias You Gotta Know.
The Bread and Butter
We summarize some key topics from the following readings, Tintinalli (7e) Chapter 280, 295 ; Rosen’s 8(e) Chapter 50 – a well written chapter, but, the point isn’t to just take our word for it. Go enrich your fundamental understanding yourself!
Atrial Fibrillation
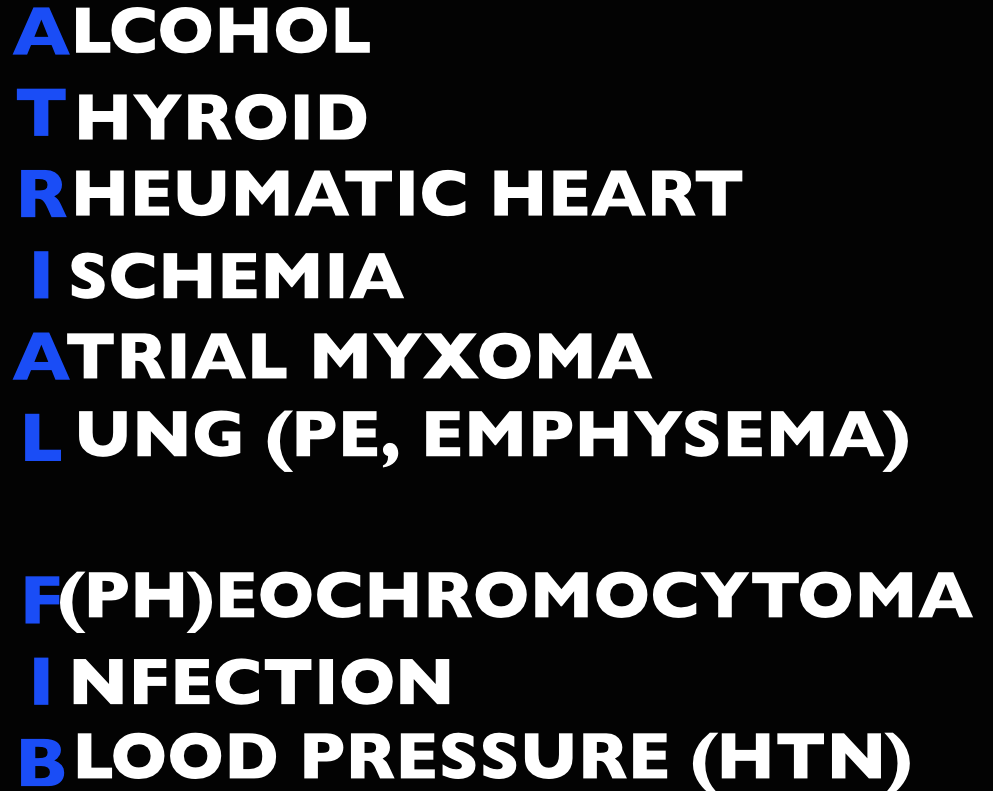
Etiology
Management
Unstable (hypotension, pulmonary edema, altered mental status, chest pain) – cardioversion.
- Pads in either an anterior-lateral (AL) or anterior-posterior (AP) position followed by synchronized cardioversion at 100-200 J biphasic. Current literature shows no significant difference in pad placement [1]
- If cardioversion fails, try amiodarone load or diltiazem. Check out EMCrit on Crashing A Fib
Stable
- Rate control. A target of <120 beats per minute is acceptable in the ED [2-3]. First line agents are nodal blocking agents such as diltiazem and metoprolol
- Diltiazem 0.25 mg/kg IV over 2 minutes with a peak effect in 2-7 minutes. Can repeat at 0.35 mg/kg IV over 2 minutes.
- Metoprolol 5-10 mg IV.
- Rhythm control with cardioversion. While there’s no proven benefit to rhythm control, many patients would prefer to be in sinus rhythm and ED cardioversion of stable new-onset atrial fibrillation is appropriate in a select population, notably, when the onset is <48 hours (or <72 hours per Rosen). The pooled literature suggests a thromboembolism rate <0.8% [4].
- Note: A recent article in JAMA by Nuotio et al found a higher rate of embolic events in patients who were electively cardioverted after >12 hours in atrial fibrillation.The 30 day risk of thromboembolism when cardioverted between 12-48 hours was 1.1%, compared to the ~2% risk if cardioverted after 48 hours. While the risk is still small, it is higher than the ~0.3% risk of thromboembolism with anticoagulation on board.
- Treat the underlying cause (ex: sepsis, pulmonary embolism, hyperthyroidism, etc)
- May also consider Amiodarone, Digoxin (mean >11 hours to rate control) [3]
In atrial fibrillation with pre-excitation (WPW), an often wide and irregular rhythm with different/changing morphologies to the QRS do NOT treat with an AV Nodal blocking agent as this may result in death (Adenosine, Beta-blocker, Calcium-channel blocker, etc). Treat with procainamide or shock
Disposition – Admit patients that present unstable, with underlying co-morbidities, or those that are not rate controlled. Depending on the patient’s follow up and local practice patterns, the
Atrial Flutter
How to Avoid Misdiagnosing Atrial Flutter – Dr. Amal Mattu
Management – same as atrial fibrillation
- More sensitive to electrical cardioversion, less sensitive to chemical cardioversion
Multifocal Atrial Tachycardia
Irregular narrow complex tachycardia with p waves of at least 3 morphologies (this can be difficult to see, so look in multiple leads, particularly V2)
Etiology -often seen in advanced pulmonary disease
Management – Treat the underlying cause, do NOT cardiovert MAT
Learn from the master ECG educator, Dr. Amal Mattu
Generously Donated Rosh Review Questions (Scroll for Answers)
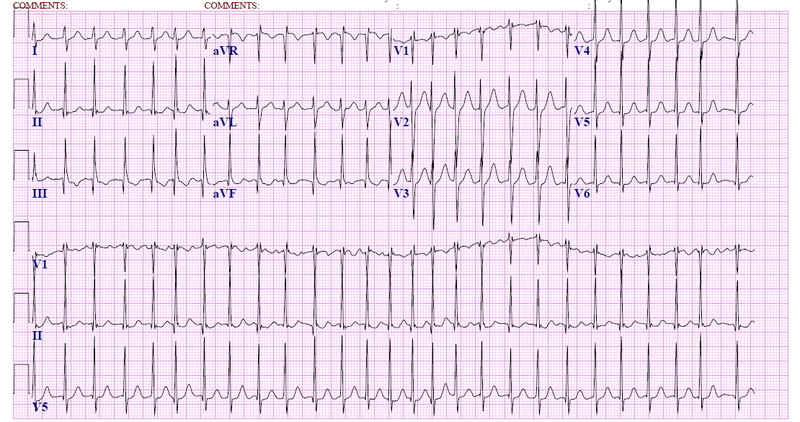
Question 1. A 72-year-old man with a history of hypertension, diabetes, and congestive heart failure presents to the ED with heart palpitations for the past 4 days. He denies any chest pain, shortness of breath, abdominal pain, or history of similar palpitations. In the ED, his vital signs are BP 135/75, HR 138, RR 14, and oxygen saturation 98% on room air. His ECG is seen below. Which of the following is the most appropriate next step in management?
A. Chemical cardioversion
B. Rate Control
C. Synchronized cardioversion
D. Warfarin
Question 2. When do you worry about giving calcium channel blockers, beta-blockers, or digoxin in a patient with atrial fibrillation?
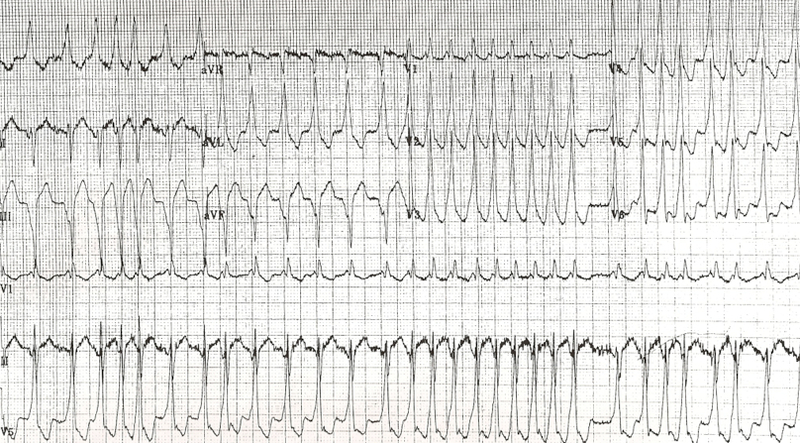
Question 3. An 18-year-old woman presents with palpitations and near syncope. Her vitals are T 98.7F, HR 199, BP 113/66, RR 32, and oxygen saturation 94%. Her ECG is shown below. What treatment is indicated?
A. Administer adenosine 6 mg IV
B. Administer diltiazem 10 mg IV
C. Administer lopressor 10 mg IV
D. Administer procainamide 100mg IV
References
1. Kirkland S, Stiell I, AlShawabkeh T, Campbell S, Dickinson G, Rowe BH. The Efficacy of Pad Placement for Electrical Cardioversion of Atrial Fibrillation/Flutter: A Systematic Review. Acad Emerg Med. 2014;21(7):717–726.
2. Chapter. Rosen’s Emergency Medicine, 8e.
3.Chapter. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 7e. New York, NY: McGraw-Hill; 2011
4. Cohn BG, Keim SM, Yealy DM. Is Emergency Department Cardioversion of Recent-onset Atrial Fibrillation Safe and Effective? J Emerg Med. 2013;45(1):117–27.
Answers
1. B. Atrial fibrillation is caused by chaotic, disorderly firing from a second focus within the atria, resulting in uncoordinated atrial contractions. Patients with atrial fibrillation may present with palpitations, chest pain, shortness of breath, or they may be asymptomatic. Atrial fibrillation can be classified as chronic or paroxysmal, with paroxysms lasting minutes to days. On ECG, there are irregularly irregular narrow QRS complexes. In addition, no discernible p-waves are noted, rather fibrillatory waves are seen. Unless the patient is hemodynamically unstable, the mainstay of therapy is rate control. This is achieved through medications that act on the AV node such as calcium channel blockers (eg diltiazem or verapamil), beta-blockers, or digoxin. Due to digoxin’s slow onset of action and side effects, it is considered a second line medication.
If atrial fibrillation has been present for >48 hours, there is an increased risk of atrial thrombus formation. An echocardiogram should be obtained in these patients to exclude thrombus formation prior to rhythm control. Patients with chronic atrial fibrillation usually are placed on warfarin (D) or a similar anticoagulant to prevent thromboembolism.Chemical cardioversion (A) (amiorodone, procainamide or flecainide) can be attempted in patients with paroxysmal atrial fibrillation for less than 48 hours. Synchronized cardioversion (C) is used in patients who are hemodynamically unstable. This can be achieved by administering 50 – 100 J of electricity in synchronization mode.
2. If a patient has an accessory pathway, such as Wolff-Parkinson-White Syndrome.
3. D. This patient presents with near syncope in the setting of atrial fibrillation with abberant conduction most likely secondary to Wolff-Parkinson-White (WPW) syndrome and should be chemically or electrically cardioverted. WPW syndrome refers to the presence of an accessory pathway between the right atrium and right ventricle. This accessory pathway has a shortened refractory period and can bypass normal conduction down the AV node. Because of the shortened refractory time, the accessory pathway in WPW can conduct atrial impulses much faster than the AV node can allowing for a ventricular rate between 150 and 300 beats per minute. Any tachycardia greater than 200 beats per minute in an adult should raise suspicion for an accessory pathway.
Patients with WPW can be asymptomatic or may present with severe tachydysrhythmias. The most common presenting dysrhythmia is reentrant tachycardia (70-80%) and second is atrial fibrillation (10-30%). In these tachydysrhythmias, the patient can conduct orthodromically (down the AV node and back up the accessory pathway), antidromically (down the accessory pathway and up the AV node) or in both directions. Patients who have any antidromic conduction will present with wide complex tachycardias. In patients with irregularly irregular wide-complex tachycardias, atrial fibrillation with WPW is the most common diagnosis. If the patient is unstable, electrical cardioversion should be pursued immediately as these patients run the risk of degrading into ventricular tachycardia and ventricular fibrillation. If the patient is stable, procainamide can be administered for chemical cardioversion. Procainamide is a class Ia anitdysrhythmic agent. The dose of procainamide (D) is 18-20 mg/kg administered at a rate of 20-30 mg/min.

In patients with WPW, antidysrhythmic agents that block the AV node are contraindicated. Blocking the AV node causes unopposed electrical conduction down the accessory pathway. This can lead to ventricular dysrhythmias. Additionally, the accessory pathway in WPW responds paradoxically to AV nodal blocking agents by further decreasing its refractory time. Adenosine (A), beta-blockers (C), calcium-channel blockers (B) and digoxin all block the AV node.
2 thoughts on “Episode 15 – Atrial Fibrillation/Flutter”
Comments are closed.