iTunes or Listen Here
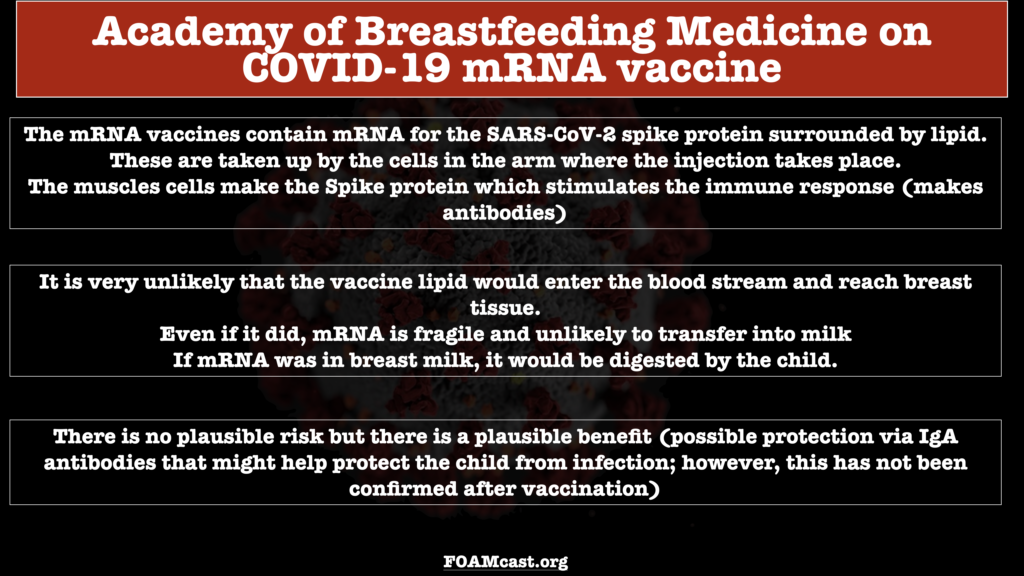
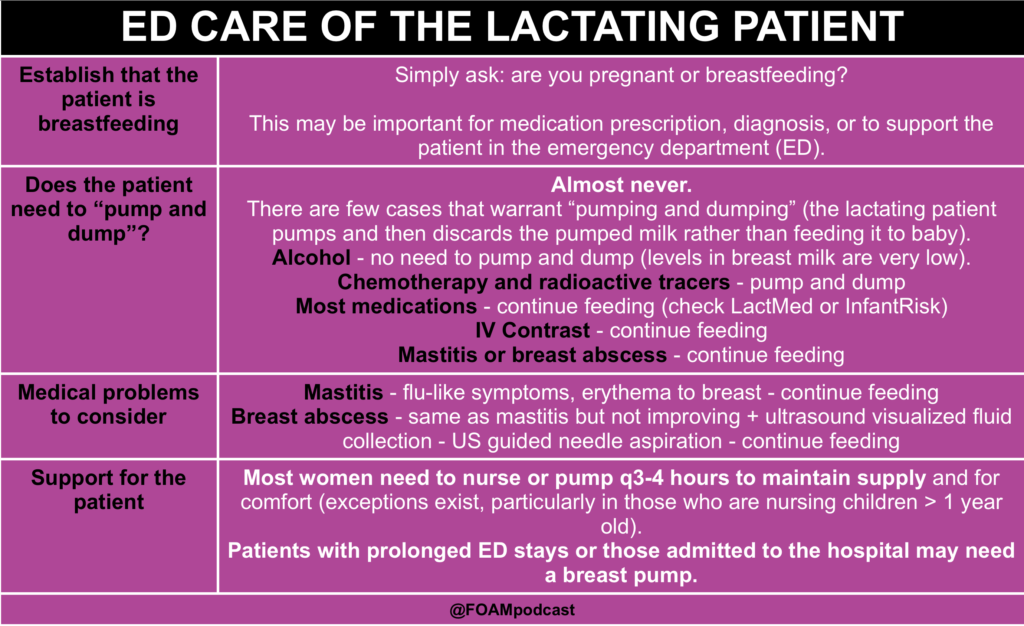
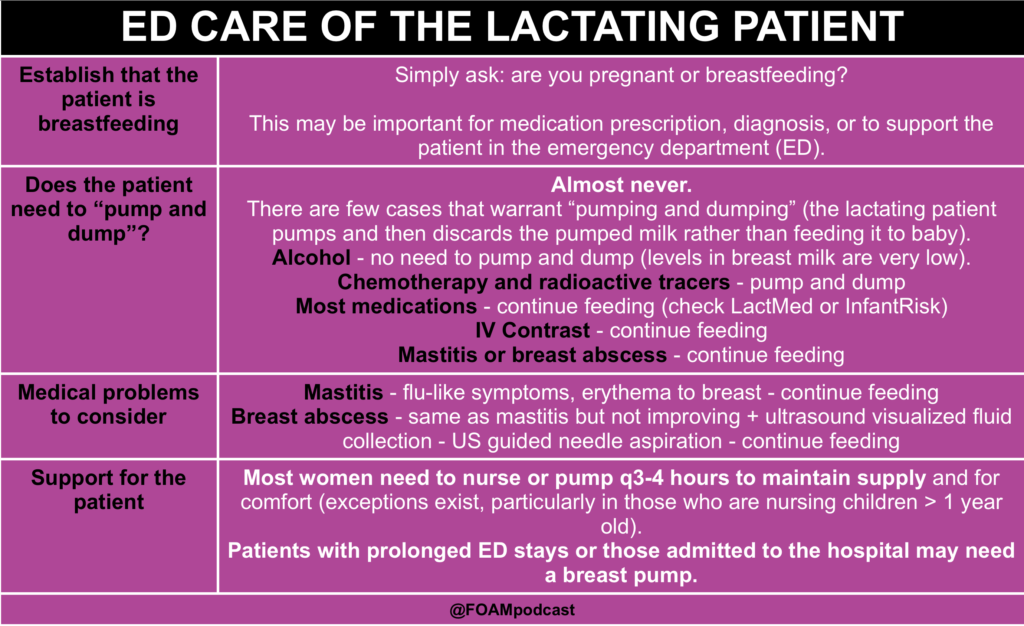
Emergency providers receive training to care for pregnant patients but little training to care for breastfeeding patients. Many myths persist, particularly urging patients to “pump and dump” (pump and discard milk instead of feeding the baby) after medications or illness that are, in fact, completely safe to continue breastfeeding through . We review popular medications used in the emergency department (ED) as well as other pearls regarding the ED care of lactating patients (references for drugs come from LactMed, other references are listed at bottom of page).
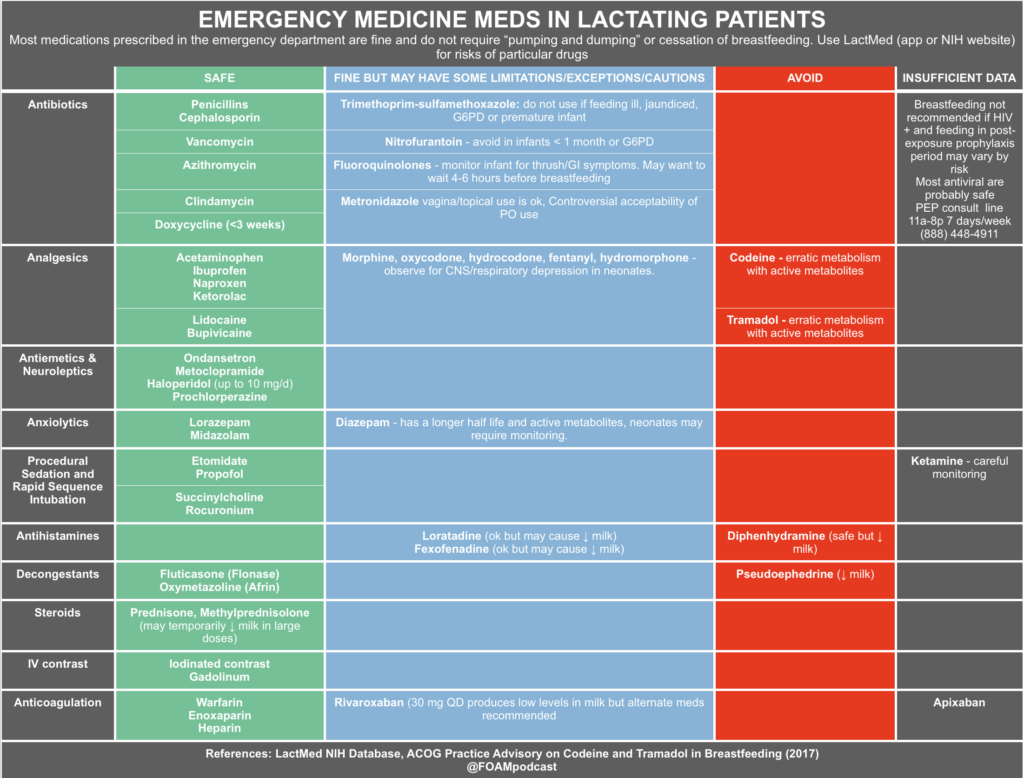
Medications During Breastfeeding
We often obsess over medications that are safe in pregnancy but may not have much of an idea of what medications are ok in patients who are breastfeeding. Rare medications are unsafe in breastfeeding (chemotherapy, radioactive isotopes) but most that we prescribe in the emergency department are fine (including anesthesia/procedural sedation meds – see this Anesthesia graphic). Please review medications prior to prescribing to ensure that they are safe for the infant and will have no deleterious effects on lactation. For example, pseudoephedrine, a seemingly benign medication, can dry up a patient’s milk supply.
LactMed is a searchable database provided by the National Institutes of Health that summarizes the safety of medications in breastfeeding and the effects of medications on lactation. There is also a free LactMed app. Providers and patients can also call InfantRisk( 806) 352-2519 regarding specific medications (Mon-Fri 9am-6pm CST)
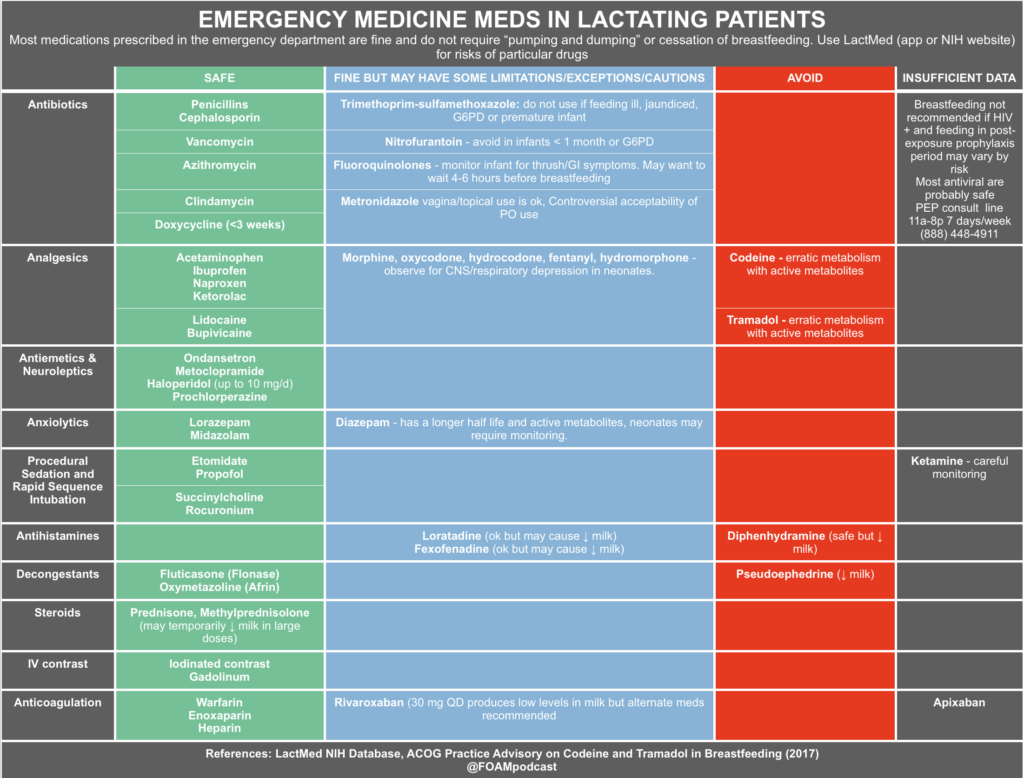
**Note: Some sources cite different safety profiles so we have tried to synthesize this information but depending on the patient and the source, the risk profile may be a bit different.
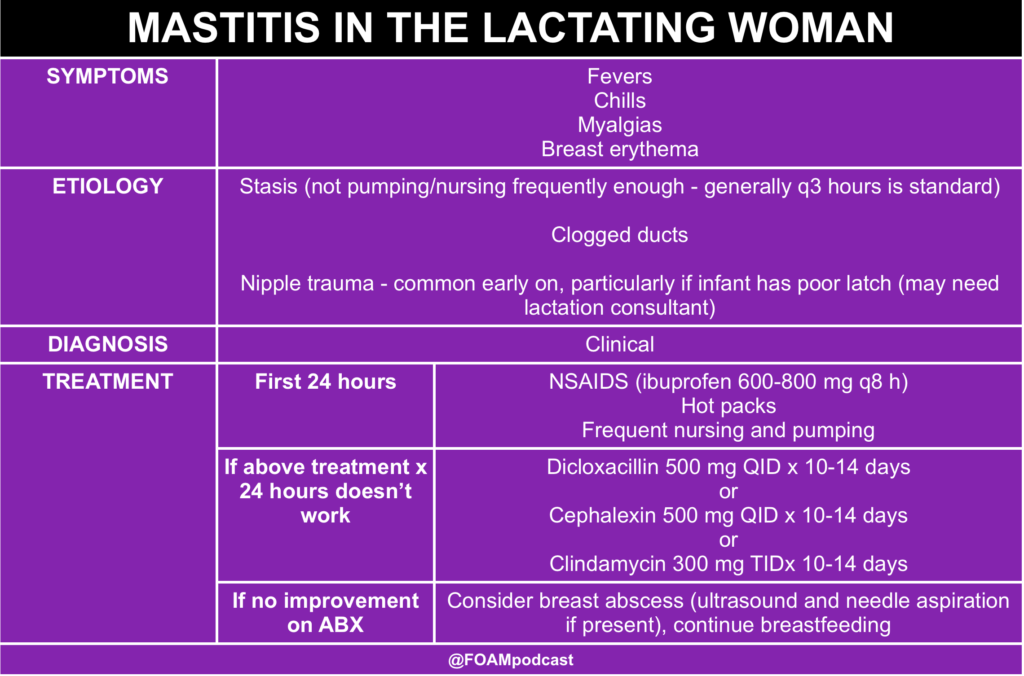
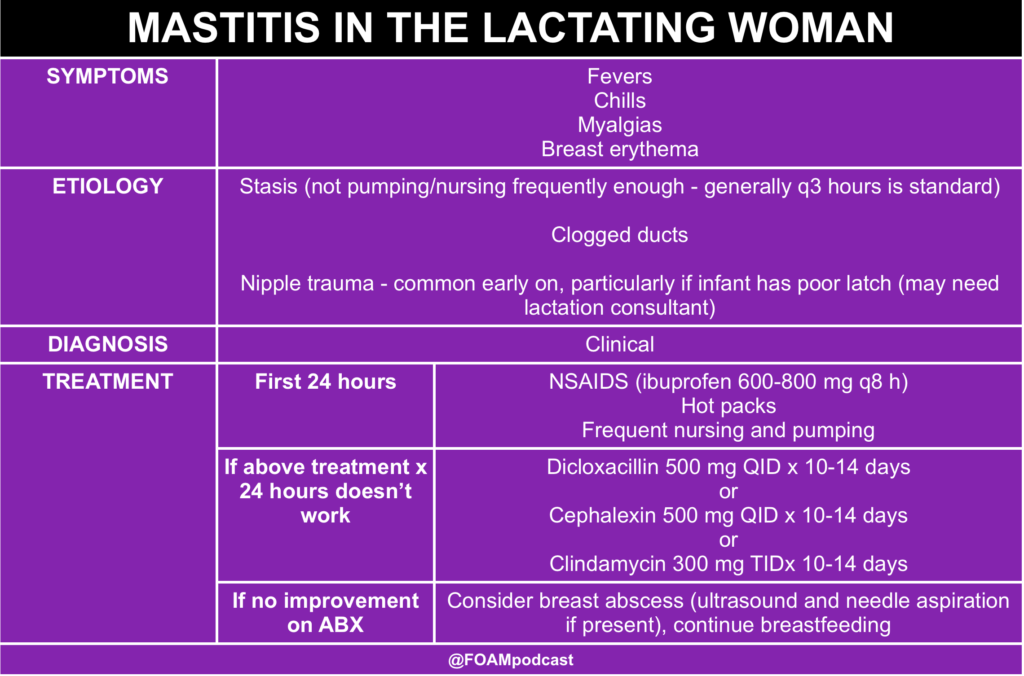
Medical illnesses specific to the lactating patient
General support for the lactating patient
Thanks to the physicians and lactation experts of Dr. Milk (@DoctorDrMilk) for providing peer review.
Rosh Review Emergency Board Review Questions
A 36-year-old woman presents to the office for a painful right breast for the past two days. She is one month postpartum. The patient reports swelling and redness of the right breast in addition to pain. She is febrile to 101.2°F. On physical examination, the lower lateral quadrant of the right breast is erythematous, firm, warm, and markedly tender to palpation. Enlarged right axillary lymph nodes are noted on exam. In addition to warm compresses, which of the following would be the most appropriate course of treatment?
A. Cease breastfeeding from the affected breast
B. Incision and drainage
C. Initiation of dicloxacillin 500 mg four times daily
D. Initiation of trimethoprim-sulfamethoxazole 800 mg-160 mg two times daily
[accordion]
[toggle title=”Answer” state=”closed”]
C. Initiation of dicloxacillin 500 mg four times daily is the treatment of choice for postpartum women with lactational mastitis who do not have a penicillin allergy. Mastitis is an infection of the breast commonly seen in breastfeeding women from milk duct blockage, prolonged breast engorgement, and nipple trauma. The most common bacterial pathogen implicated in mastitis is Staphylococcus aureus. Patients most commonly complain of a swollen, painful, red breast. Diagnosis is a clinical one, but a breast milk culture can be performed in severe infections or infections refractory to initial treatment. For worsening symptoms or infection that is not responsive to usual treatment, an ultrasound of the breast may be indicated to rule out a breast abscess. Treatment includes analgesics, warm compresses, and continued emptying of the breast. Antibiotic choice includes dicloxacillin, cephalexin, or clindamycin (if penicillin-allergic). For individuals with increased risk of methicillin-resistant S. aureus (MRSA), clindamycin or trimethoprim-sulfamethoxazole can be used. Sulfa-containing drugs should not be used in mothers who are nursing newborns due to risk of kernicterus.
[/toggle]
[/accordion]
References:
- Dobiesz VA, Robinson DW. “Drug Therapy in Pregnancy.” Rosen’s Emergency Medicine: Concepts and Clinical Practice. 9th ed. Chapter 180; p 2277-2295.e3
- Breastfeeding and Maternal Medication Recommendations for Drugs in the Eleventh WHO Model List of Essential Drugs
- Manual on Contrast Media. American College of Radiology. 2017
- Briggs GG, Freeman RK, Yaffe SJ. Drugs in Pregnancy and Lactation: a reference guide to fetal and neonatal risk. 8th ed. Philadelphia: Lippincott Williams & Wilkins; 2008
- Practice Advisory on Codeine and Tramadol for Breastfeeding Women. American College of Obstetrics and Gynecology. April 27, 2017.
- Hang BS. “Breast Disorders.” Tintialli’s Emergency Medicine. 8th ed. Chapter 104.
- Haastrup MB, Pottegård A, Damkier P. Alcohol and breastfeeding. Basic Clin Pharmacol Toxicol. 2014;114(2):168-73.