iTunes or Listen Here
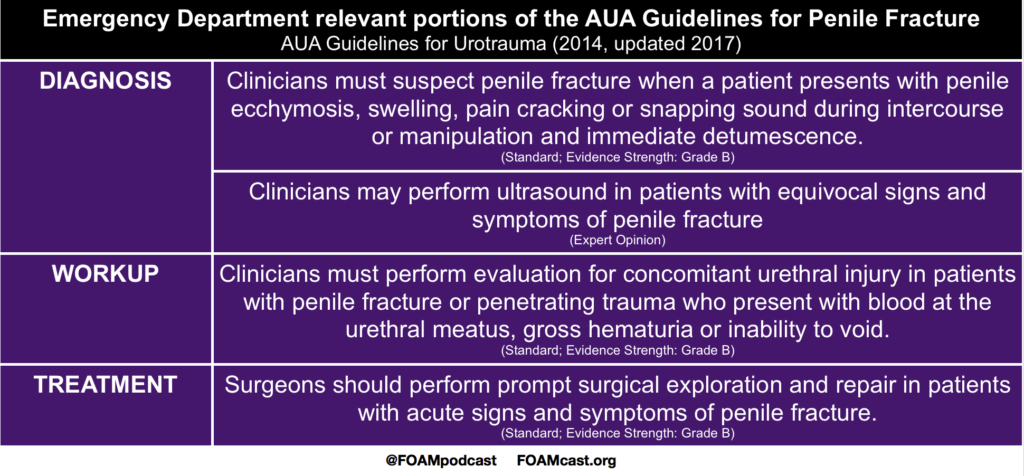
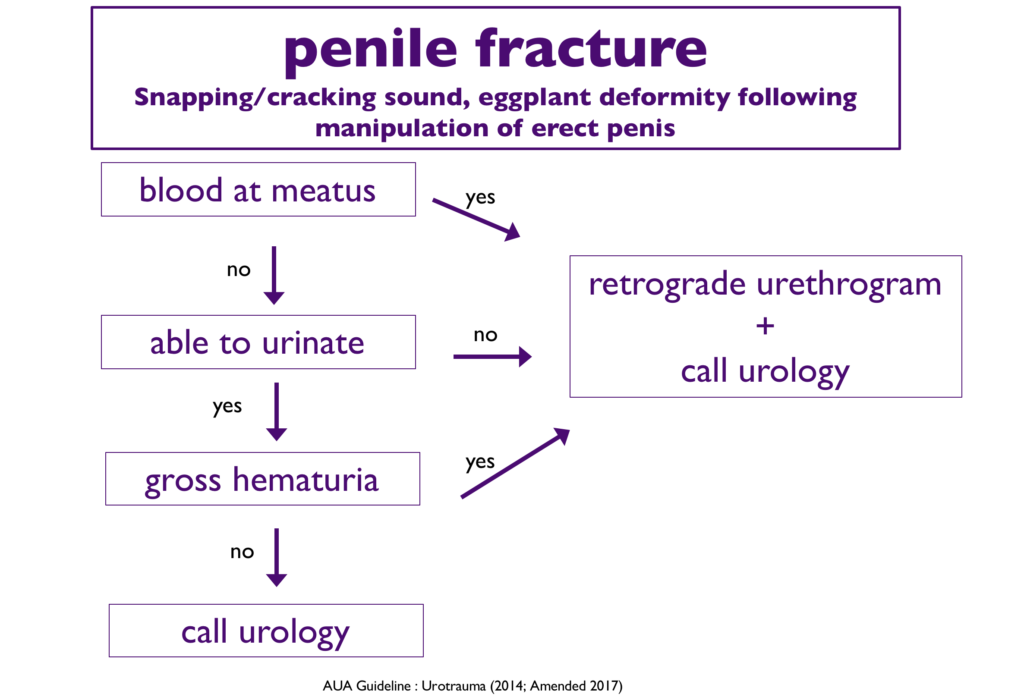
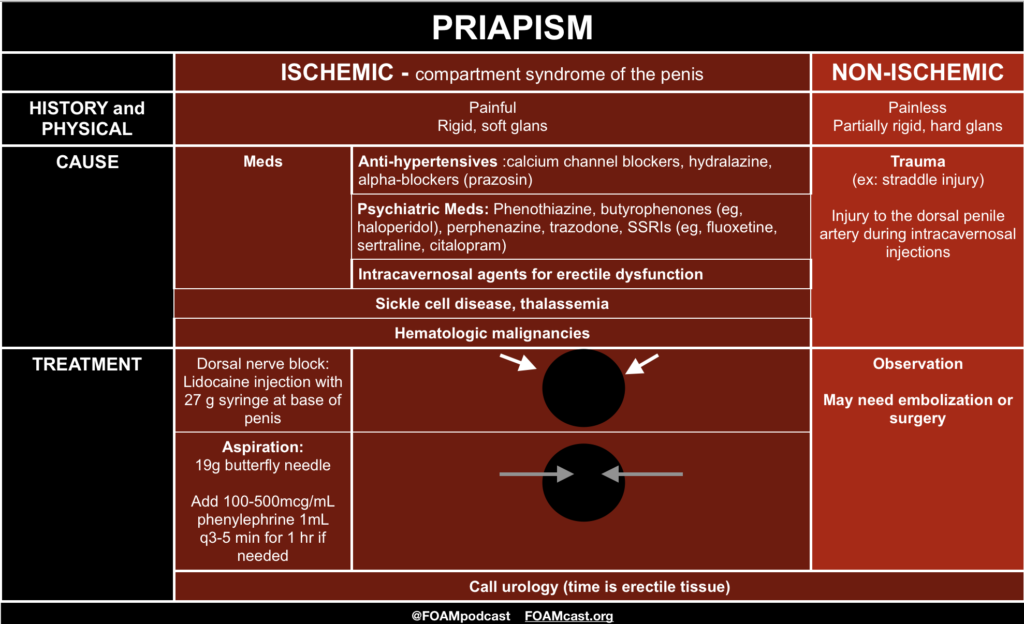
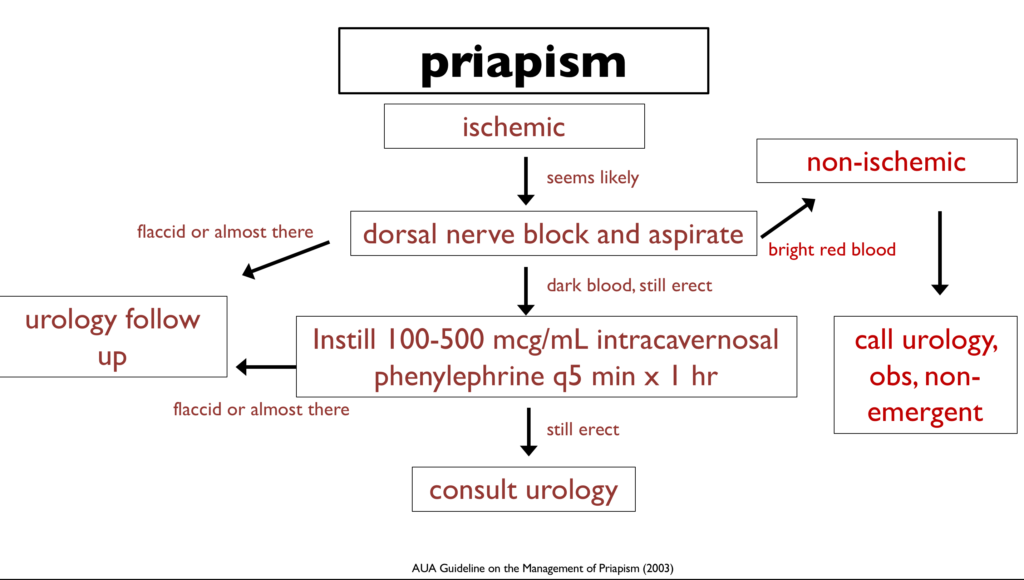
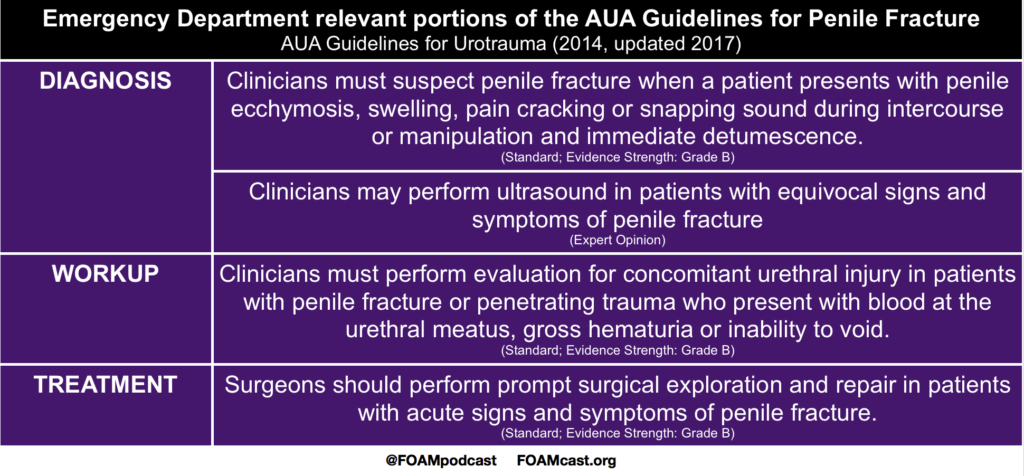
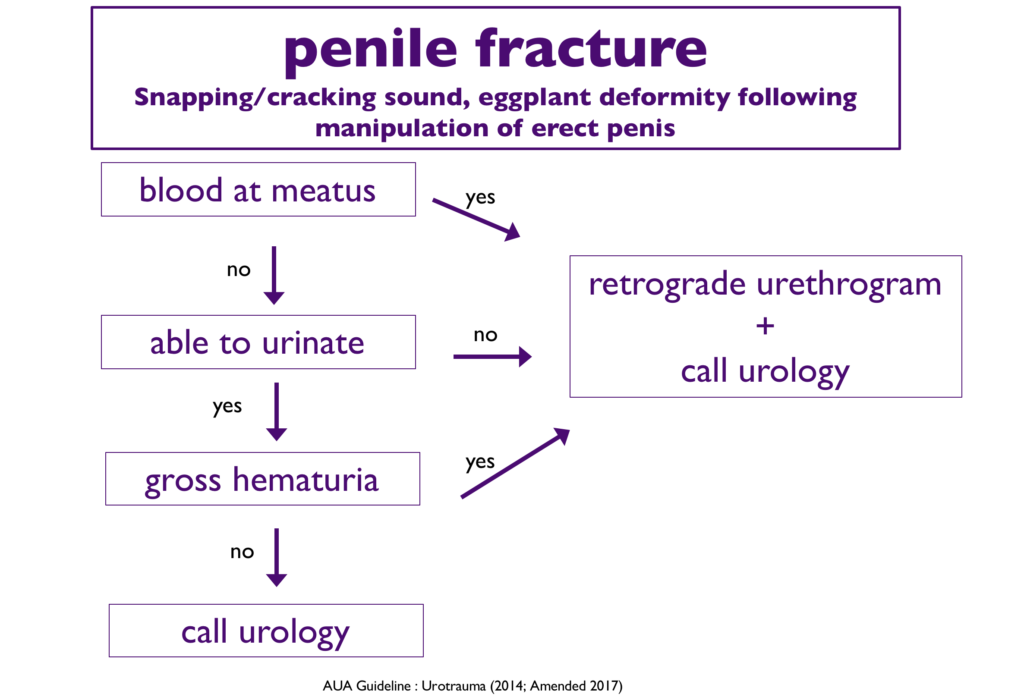
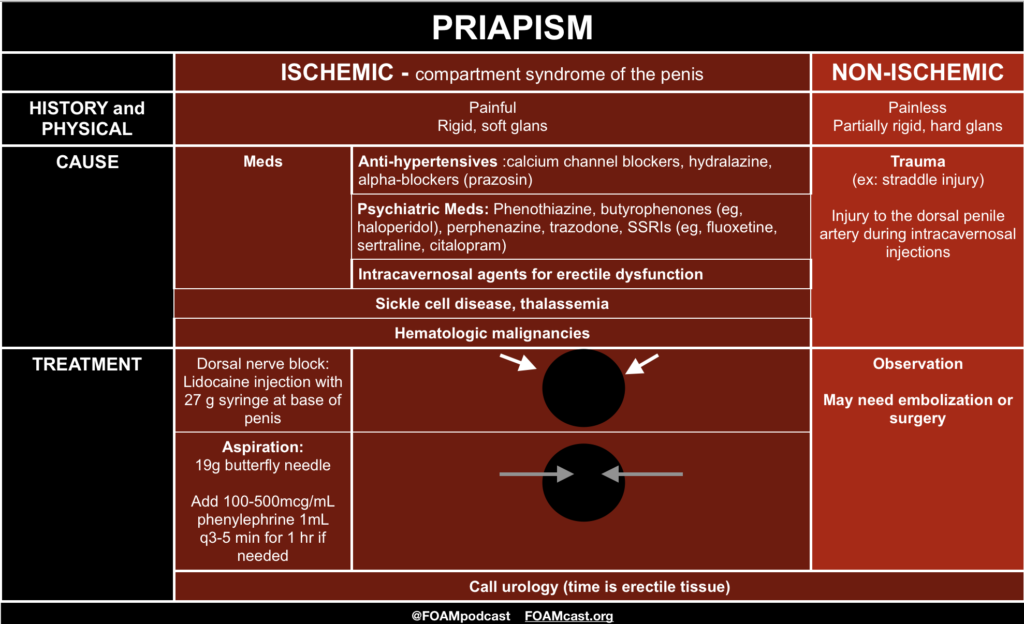
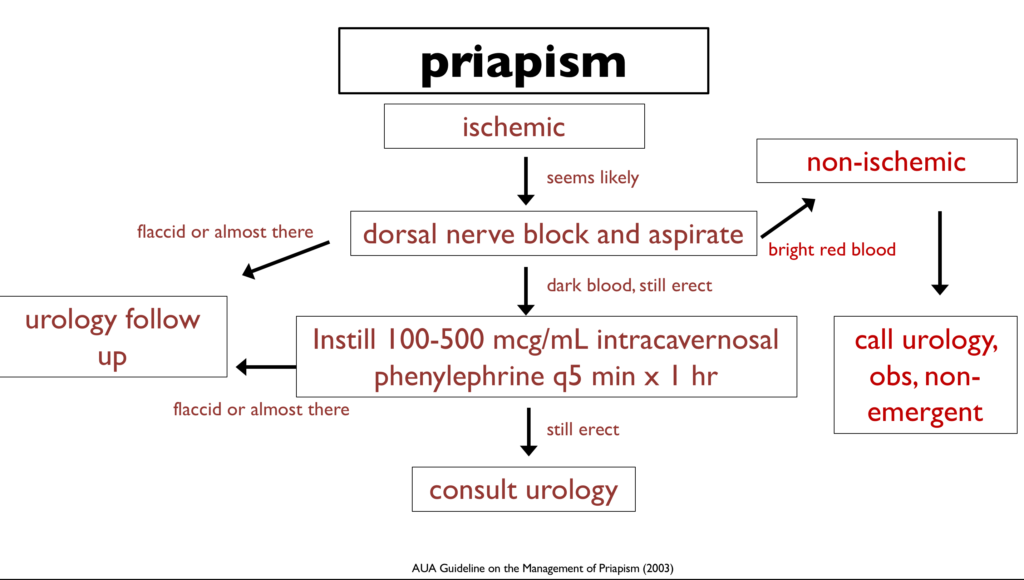
We review the American Urological Association guidelines on penile fracture and priapism. We supplement this with core content from Tintinalli and Rosen’s.
Rosh Review Emergency Board Review Questions
A 16-year-old boy with sickle cell disease presents to the emergency department having intermittent but frequent short and painful erections. He denies current pain but reports having had four unwanted painful erections beginning this morning, each becoming progressively longer with the most recent lasting one hour. On exam he is well appearing and in no distress with a flaccid non-tender penis on genitourinary exam. Which of the following is the most appropriate next step?
A. Corporal aspiration
B. Oxygen
C. Pseudoephedrine
D. Warm penile compress
[accordion]
[toggle title=”Answer” state=”closed”]
C. Priapism is a painful erection unrelated to sexual stimulation. It is most common in sickle cell patients and is usually an ischemic, low–flow process resulting in venous stasis and sickling of cells. Irreversible tissue damage begins at six hours, so patients with a painful erection are taught to seek medical attention with erections lasting more than four hours. Optimal management is not well defined and local expert opinion may vary. Brief episodes can often be managed at home with oral analgesics, brief exercise, warm/cold compresses, or showering. Recurrent episodes of priapism such as seen in our patient are referred to as stuttering priapism which may herald a longer event. The first-line treatment for stuttering priapism is with an oral alpha-adrenergic agent such as pseudoephedrine. Patients with priapism lasting more than four hours are treated with a combination of intravenous fluids, intravenous analgesia, and emergent urology consult for corporal aspiration. Conscious sedation may be indicated depending on patient age and anxiety. Once low-flow priapism is confirmed, intracavernosal injection of an alpha-adrenergic receptor agent such as phenylephrine can help to achieve detumescence. If multiple attempts at corporal aspiration fail, a surgical shunt may be indicated.
Corporal aspiration (A) is not recommended in patients with current detumescence as in our patient. Oxygen (B) is recommended if hypoxic but has not been shown to assist in achieving detumescence. Warm penile compresses (D) are a recommended home therapy to achieve detumescence early in a painful erection but will not help between recurrent stuttering priapism.
[/toggle]
[/accordion]
A 21-year-old man presents to the Emergency Department with sudden onset penile pain that occurred while having intercourse with his wife. Physical examination reveals an angulated circumcised penis with fusiform swelling and ecchymosis. Which of the following is the next best step in management?
A. Analgesic therapy and outpatient urology follow up
B. Foley catheter placement
C. Intracavernosal phenylephrine injection
D. Urologic consultation for surgical repair
[accordion]
[toggle title=”Answer” state=”closed”]
D. A urologic consultation for surgical repair is required to optimize functional outcome in the case of penile fracture. Penile fractures occur during direct penile trauma and involves rupture of Buck’s fascia, tunica albuginea, or corpora cavernosa. Symptoms include acute pain and swelling, angulation of the penis, and loss of erection. The penis may take on a characteristic “eggplant deformity” due to swelling and ecchymosis from extravasated blood that collects within Buck’s fascia. Complications include deep dorsal vein injury and partial or complete urethral rupture. Sexual intercourse is the most common cause, but other causes include animal bites, ballistic injuries, stab wounds, and vigorous masterbation. Management involves early surgical repair of the tunica albuginea (within 24-36 hours after the injury) to improve functionality.
[/toggle]
[/accordion]
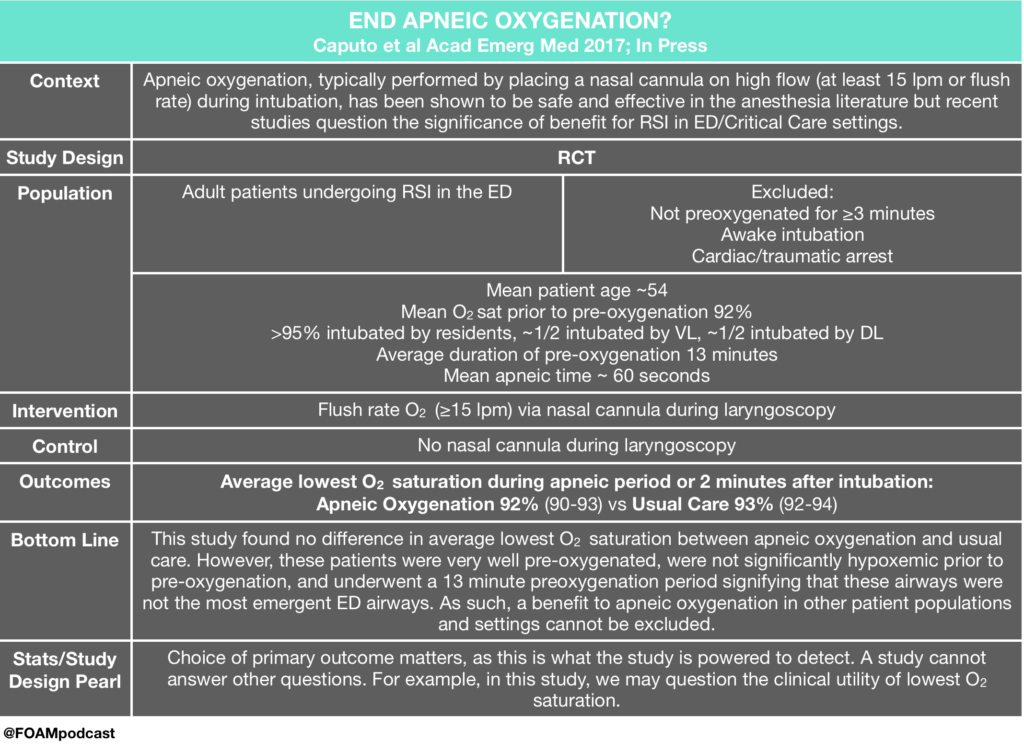
 ENDAO – Caputo et al
ENDAO – Caputo et al