Updated July 29, 2022
In a three-part series, we review the current status of the monkeypox outbreak.
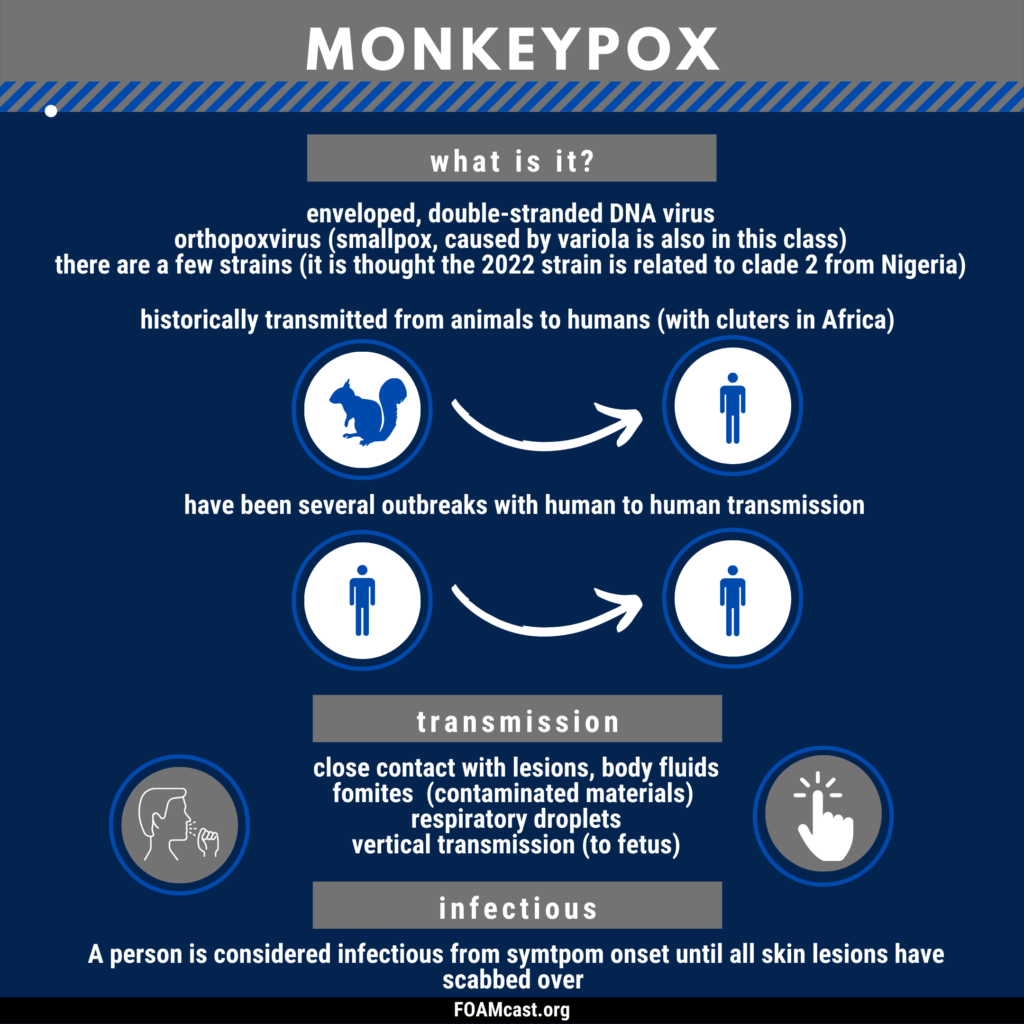
Episode 1: Virology, Transmission, Epidemiology
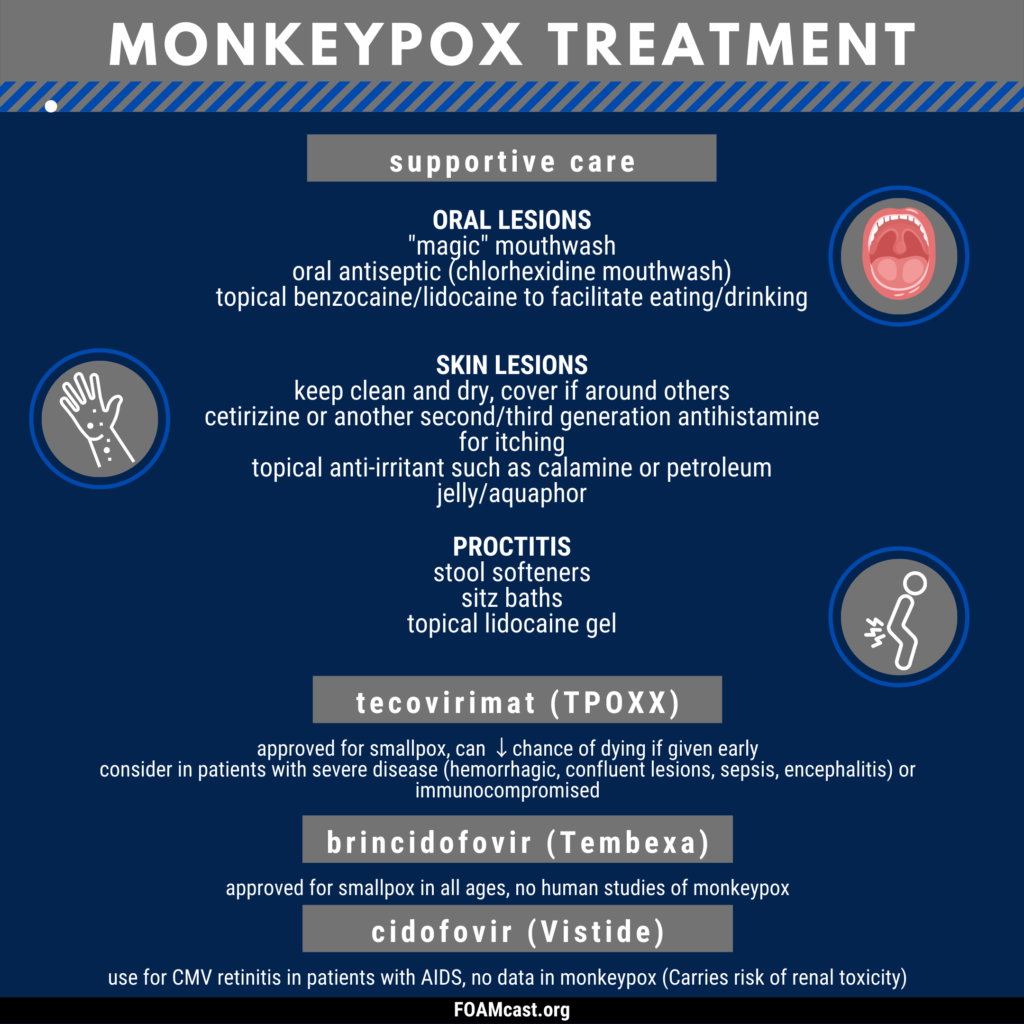
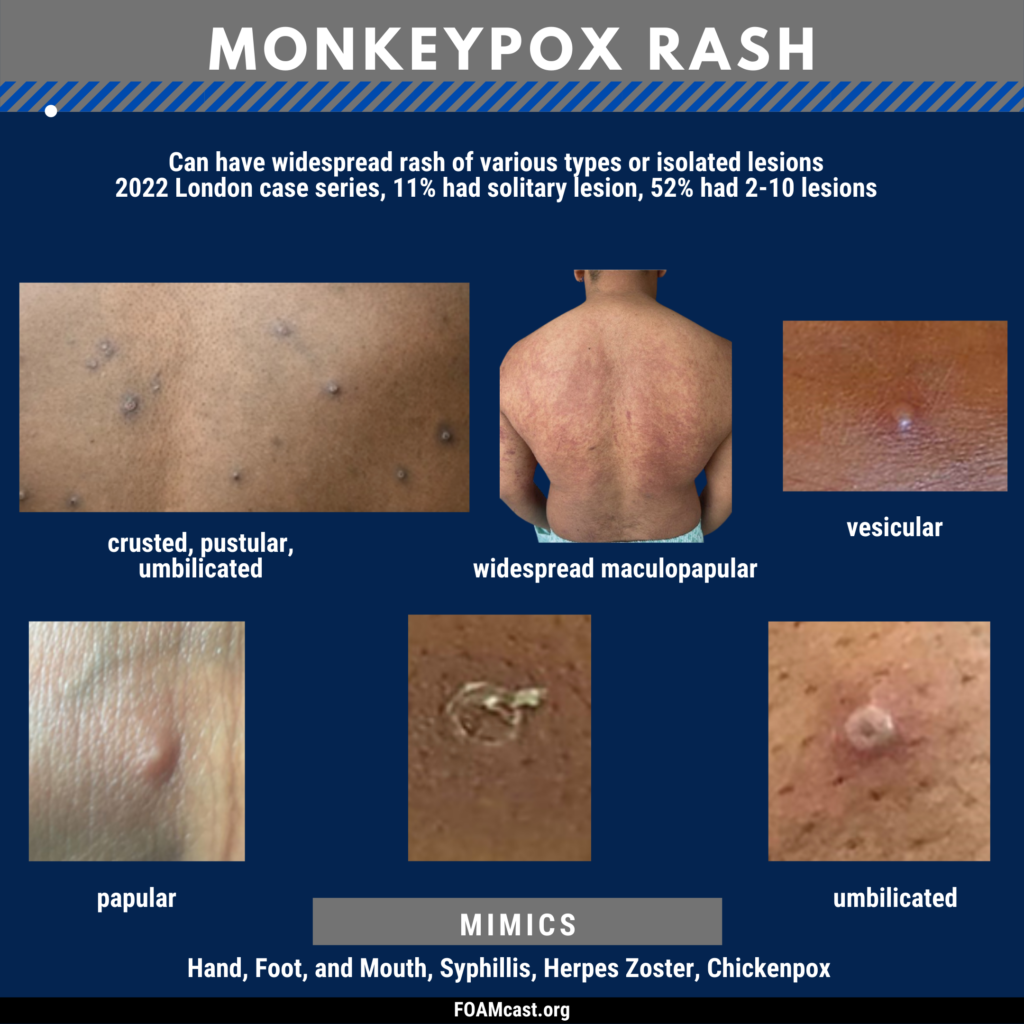
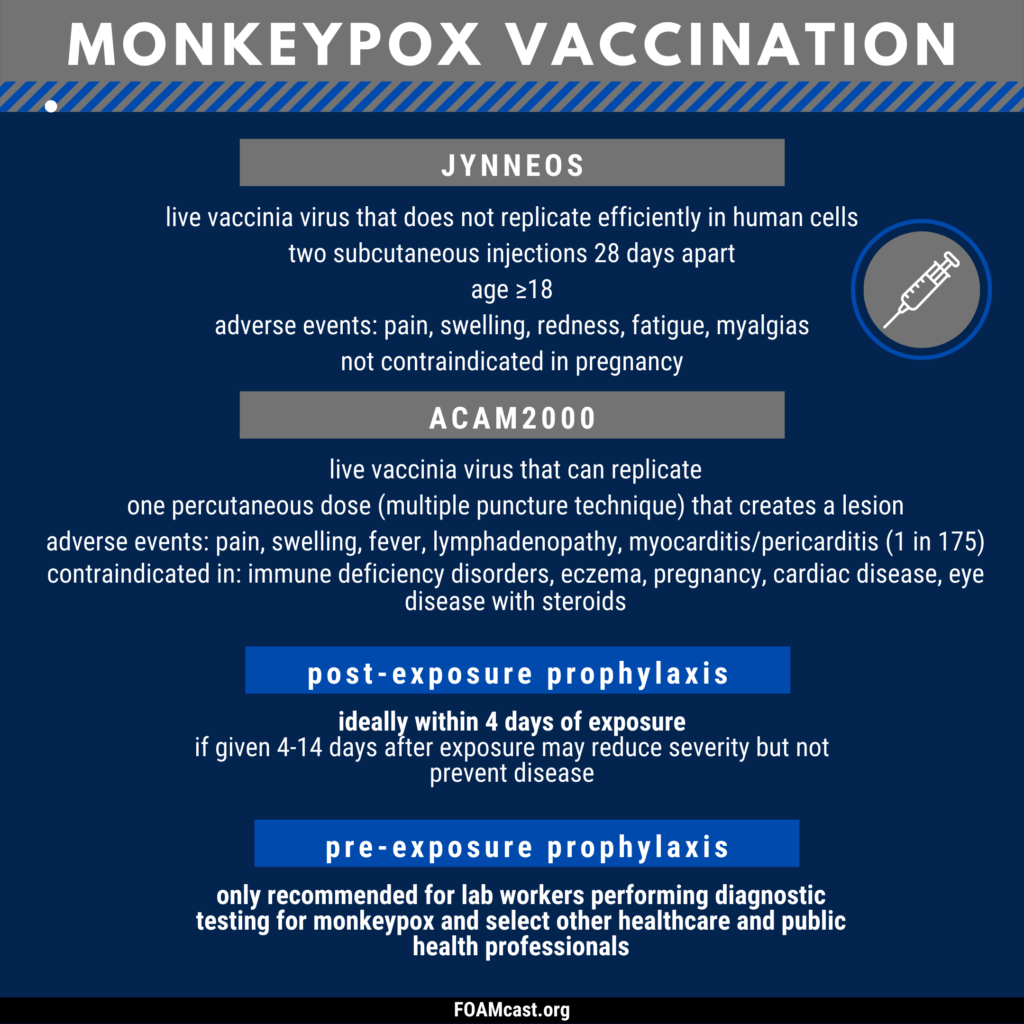
Episode 2: Clinical Manifestations, Treatment, Vaccination
Episode 3: The TLDR Quick Summary
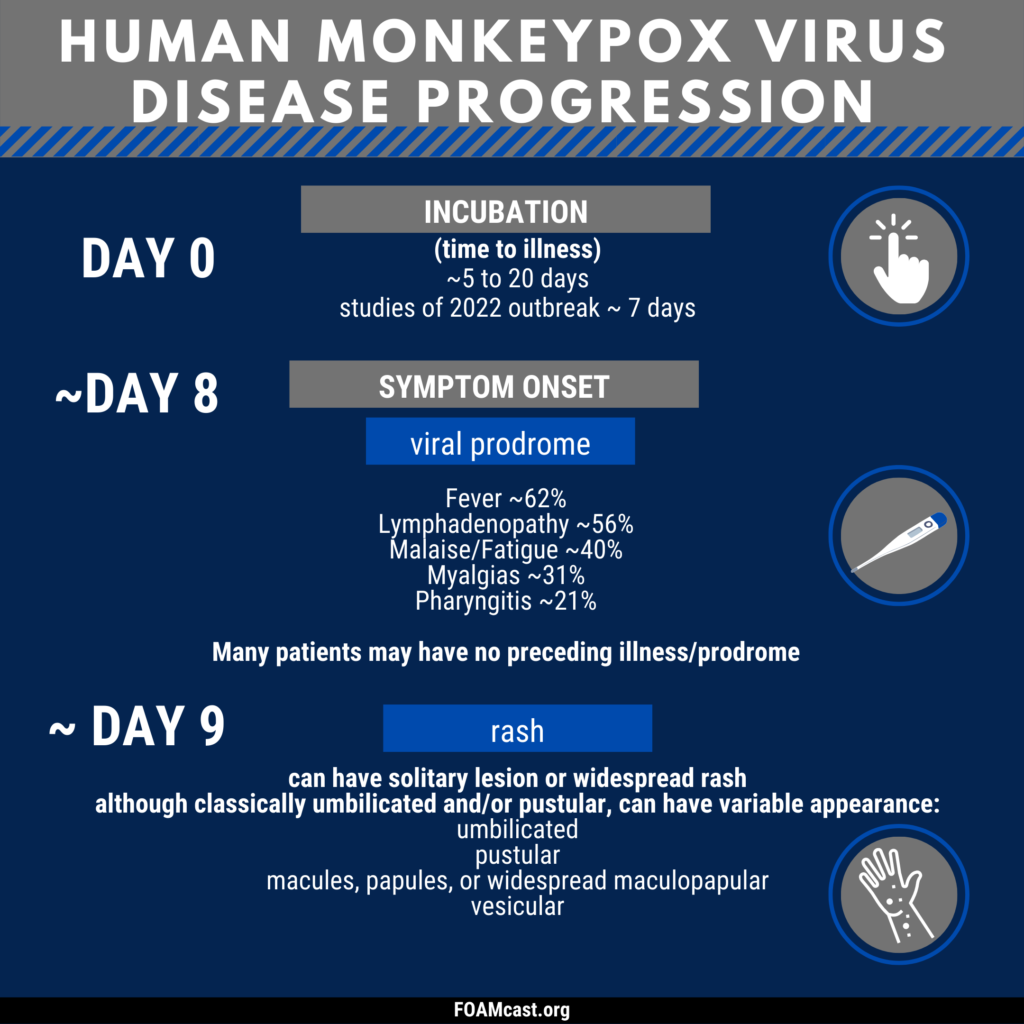
Patel A et al. Clinical features and novel presentations of human monkeypox in a central London centre during the 2022 outbreak: descriptive case series. BMJ. 2022 Jul 28;378:e072410. PMID: 35902115.
Thornhill JP et al. Monkeypox Virus Infection in Humans across 16 Countries – April-June 2022. N Engl J Med. 2022 Jul 21. doi: 10.1056/NEJMoa2207323. PMID: 35866746.