(ITUNES OR LISTEN HERE)
The Free Open Access Medical Education (FOAM)
We cover this short video from EMRAP on lateral canthotomies. This is one of those rare procedures that is vision saving; hence, it is worthy of frequent review.
Lateral Canthotomy and Cantholysis
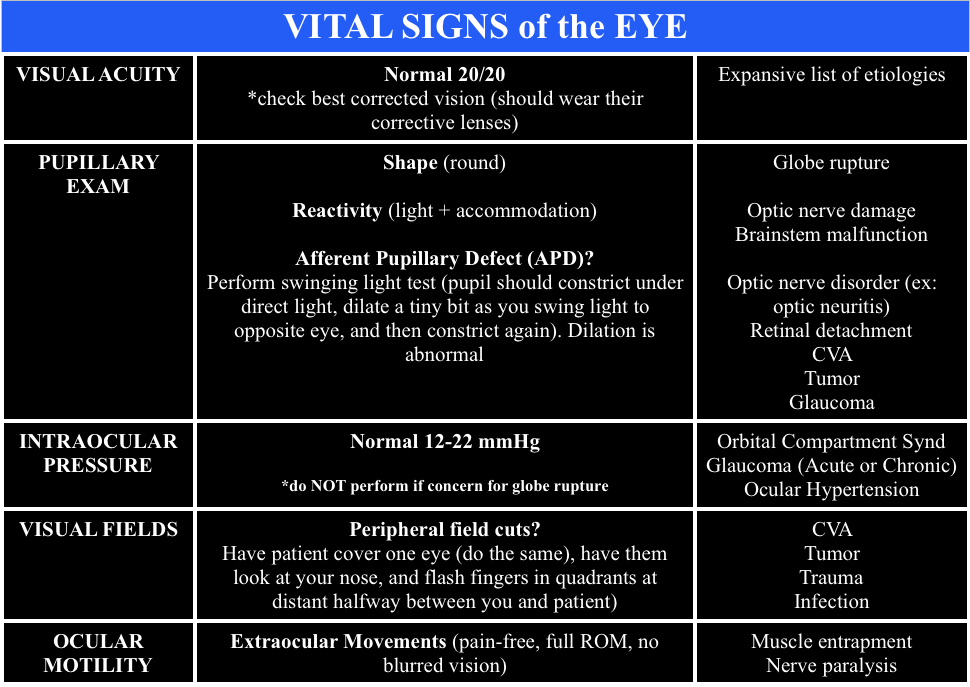
Indication: Suspect orbital compartment syndrome -afferent pupillary defect (APD), “tense eye” with taught lids, and high intraocular pressure (IOP) ≥ 40 mmHg. The APD is really a critical feature, as it is your indicator that there is optic nerve compromise from the intraorbital pressure
Clinical presentation: History of orbital trauma, often in the setting of orbital fractures with decreased visual acuity, proptosis, chemosis
Procedure: Call ophthalmology.
- Analgesia – inject lidocaine with epinephrine into the area of the lateral canthus
- Devascularize – use straight kelly clamps to crush the lateral canthus for 1-2 minutes
- Incise – Use scissors to cut the lateral canthus 1-2 cm. Then, find the inferior crus of the lateral canthus ligament (looks kind of like a wishbone from a turkey but you rarely are going to be able to see the tendon so you’re “strumming” it with the closed tips of your scissors inferomedially toward the nose) – cut the inferior crus of the ligament to release pressure (this is the key step)
When calling ophthalmology, ensure you have the “Vital Signs of the Eye”
Core Content
We delve into core content on eye trauma using Rosen’s (8th edition) Chapter 71 and Chapter 241 in Tintinalli (8th edition)
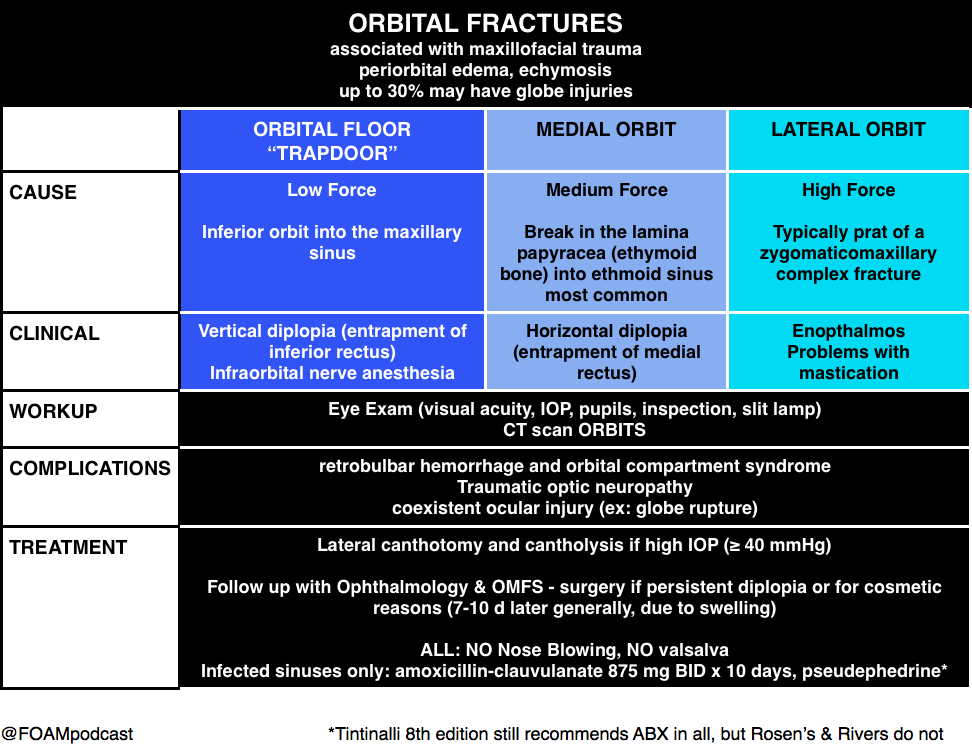
Orbital Fractures
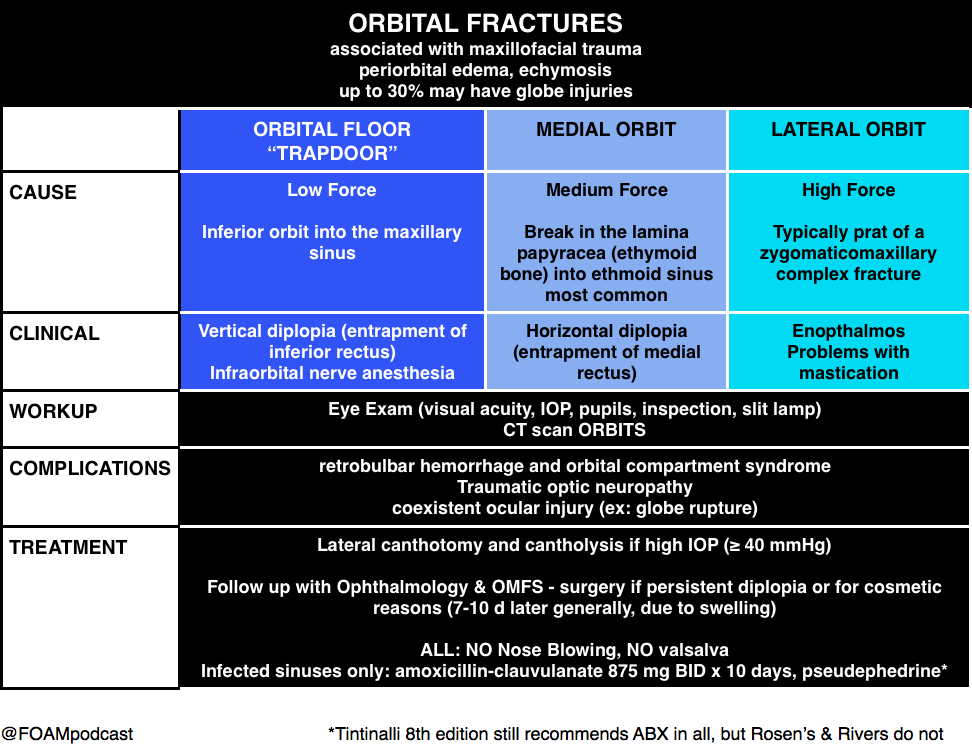
Note: entrapment is a clinical diagnosis. A CT cannot comment on function, only structure. Extraocular movements are a critical part of the fracture exam.
Pearl: young people are prone to “greenstick” fractures where the floor can actually pinch the muscle and trigger the oculocardiac reflex, which can be deadly. They often have a “white eye” without too much impressive on exam but refuse to look in a certain direction due to nausea.
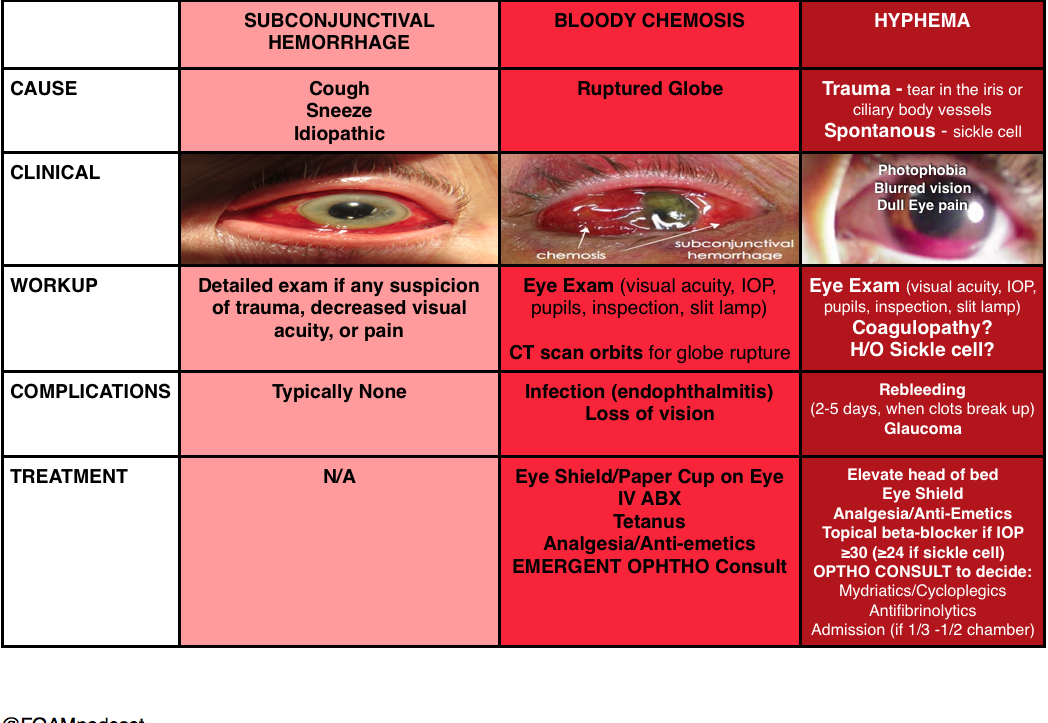
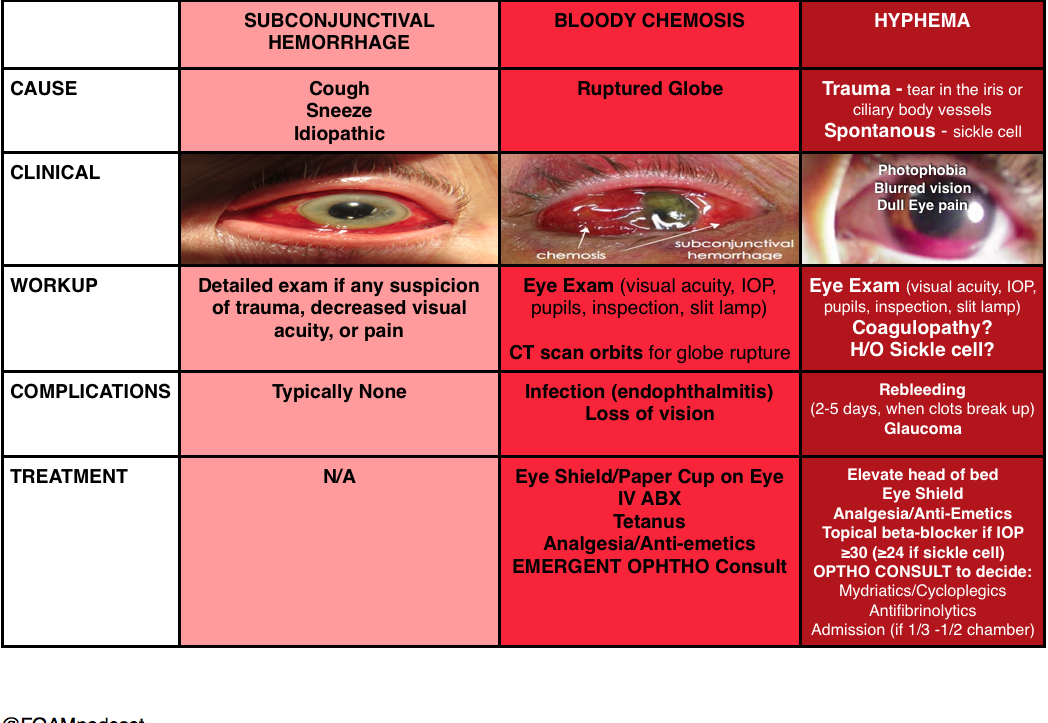
Hyphema
(and things confused with hyphema)
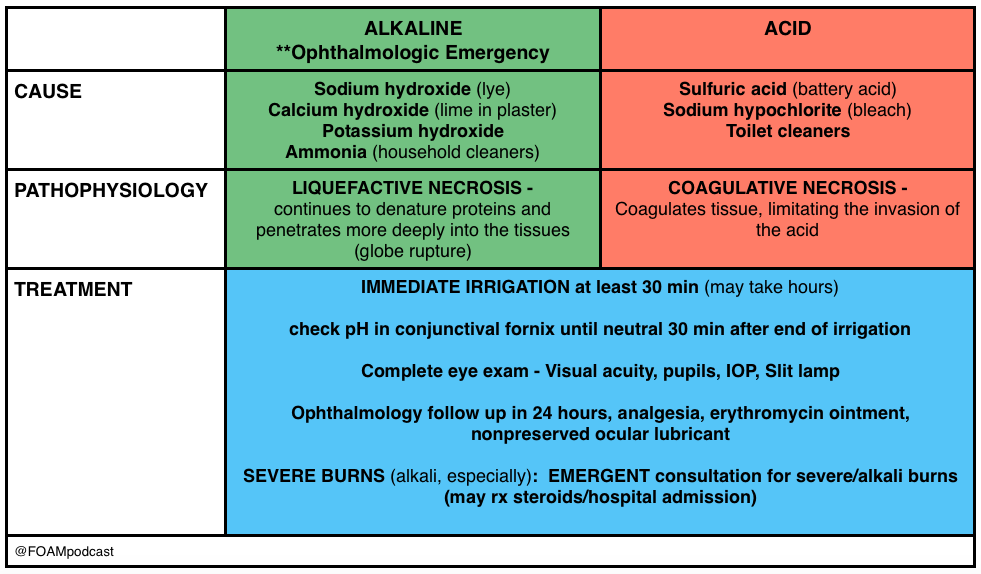
Burns
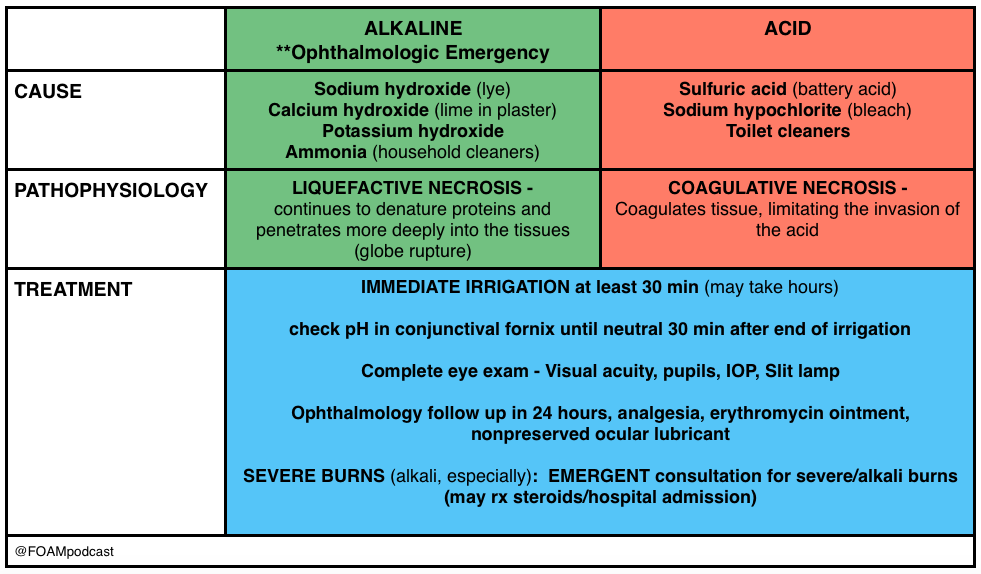
Pearl: An important thing to keep in mind is that a “white” eye after such an exposure is actually an ominous sign, as it implies ischemia of the limbal blood vessels, which portends a pretty bad prognosis. People usually think that the more red an eye, the worse when, in truth, it’s often the other way around.
Generously Donated Rosh Review Questions
A 43-year-old construction worker presents with right eye pain. He states he was using a nail gun when he felt something hit his eye. Visual examination reveals a small nail penetrating the globe. What management should be pursued?
A. CT scan of the orbit and ophthalmology consultation
B. Measure intraocular pressure and consult ophthalmology
C. Perform lateral canthotomy and consult ophthalmology
D. Remove the foreign body, start topical antibiotics and send to ophthalmology for follow up
[accordion]
[toggle title=”Answer” state=”closed”]
This patient presents with a globe injury and should have a protective shield placed, intravenous antibiotics started, CT scan of the orbit performed and ophthalmology consulted emergently. Foreign body penetration of the globe is often associated with hammering, drilling, mechanical grinding or sanding. Any patient who presents with a foreign body sensation after one of these activities should increase suspicion for a penetrating injury of the globe. CT scan, MRI and ultrasound can all be used for diagnosis but MRI should be avoided if the suspected foreign body is metal containing. Many of these patients will require operative management and should be kept NPO. A protective shield should be placed to protect the eye but patching should be avoided as it may increase pressure on the eye. Emergent ophthalmologic consultation should be obtained
[/toggle]
[/accordion]
A 23-year-old man presents after a fight. His eye is seen below. Physical examination reveals intact extraocular movements, normal fluorescein staining, normal intraocular pressure, and normal visual acuity.

What management is indicated?
A. Delayed closure
B. Laceration repair by the Emergency Physician
C. Ophthalmology consultation for repair
D. Tissue adhesive for repair
[accordion]
[toggle title=”Answer” state=”closed”]
C. Ophthalmology consultation for repair. This patient presents with a complex eyelid laceration possibly involving the canalicular system and should have a consultation with either ophthalmology or plastic surgery regarding repair. It is important to search for a penetrating globe injury in any patient with an eyelid laceration because of the proximity of structures. Simple horizontal and partial thickness lid lacerations can be repaired primarily by an Emergency Physician. However, more complicated lacerations should be considered for specialist repair because of the high likelihood of cosmetic or functional complications, or both. In general, lacerations through the orbital septum, lacerations with tissue loss, lacerations involving the lid margins, lacerations involving the levator or canthal tendons and those involving the canalicular system should be repaired by a skilled ophthalmologist or plastic surgeon. Injury to the canalicular system should be suspected in any laceration involving the medial lower eyelid. Tissue adhesive (D) is contraindicated this close to the eye and should not be used in an injury that requires precision alignment of tissue. Delayed closure (A) will likely lead to worse cosmetic outcomes. Primary repair by the Emergency Physician (B) is not recommended if the canalicular system may be involved.
[/toggle]
[/accordion]
Thanks to our peer reviewer, Michael Westafer, MD – Ophthalmologist and Glaucoma Fellow at Mayo Clinic
References
- “Eye Emergencies.” Chapter 241. Tintinalli’s Emergency Medicine: A Comprehensive Review. 8th edition.
- Sharma R and Brunette D. “Ophthalmology.” Chapter 71. Rosen’s Emergency Medicine. 8th edition, 909-930.