(ITUNES OR Listen Here)
The Free Open Access Medical Education (FOAM)
Burns are incredibly noticeable but the accompanying inhalational injury gets less attention. The amazing Maryland Critical Care Project features a neat review, N-acetylcysteine for Inhalational Burn Injury
- Occurs in ~20% of all burn patients
- Mortality is 30%
- Major mechanisms of injury:
- Temperature – often causing burns down to the level of the vocal cords, but not below.
- Toxins – products of combustion such as cyanide, carbon monoxide, and hydrogen sulfide are asphyxiants and impair oxygen utilization
- Irritants – inhaled particulates irritate airways
- Airway edema peaks at 24-48 hours
- Diagnosis made on bronchoscopy
Nebulized heparin, N-acetylcysteine, and albuterol protocol
May be beneficial, but protocols based on small studies. Rosen gives a head nod to this regimen, yet the evidence is questionable [1-3].
Nebulized heparin can be used at 10,000 international units every 4 hours, followed by nebulized NAC & albuterol 2 hours later for a total of 7 days.
- Nebulized heparin may help prevent formation of airways casts.
- NAC may have a mucolytic effect and help scavenge free radicals.
- Albuterol added to prevent bronchospasm
- Alternating nebulized heparin and NAC may:
- Improve P/F ratio (not a patient centered outcome)
- Decrease ventilator days
- Reduce the development of acute lung injury
The Bread and Butter
We cover burns including nomenclature, fluid resuscitation, burn center referral criteria, and more. We do this based on Rosen’s and Tintinalli. But, don’t just take our word for it. Go enrich your fundamental understanding yourself.
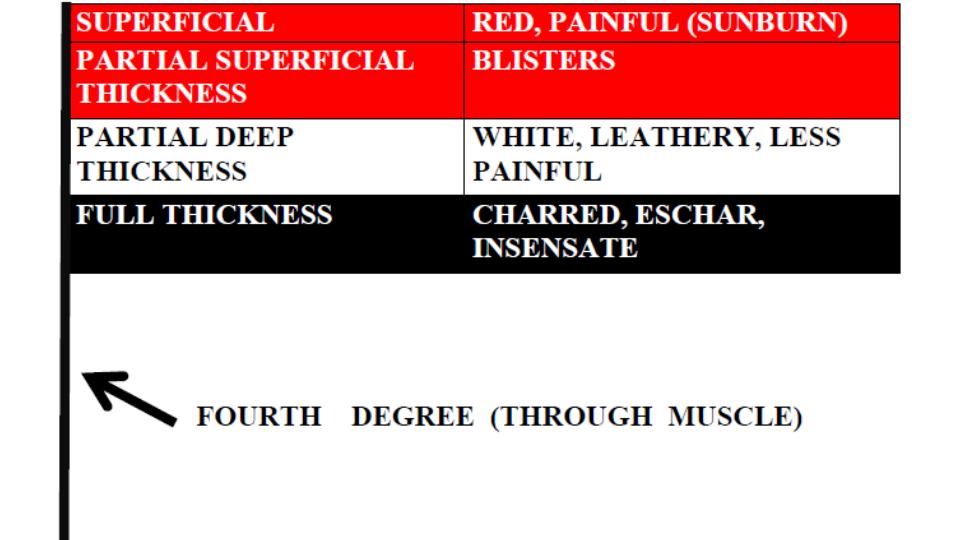
Burn Depth
Classically, burns were described in degrees but are now described by the degree of thickness (except, apparently, fourth degree burns). At FOAMcast, we like to remember these distinctions by thinking about the Egyptian flag, with the flag pole representing fourth degree burn or burns essentially down to the bone.
Fluid Resuscitation
The Parkland Formula is probably one of the most well known but both this formula and the modified Brooke formula have led to fluid “creep” or over-resuscitation, which may have lasting consequences. Major guidelines and Rosenalli approve another method, the “Rule of Tens.”
- Estimate burn size (TBSA) to the nearest 10%.
- Multiply %TBSA x 10 = Initial fluid rate in mL/hr (for adult patients weighing 40 kg to 80 kg).
- For every 10 kg above 80 kg add 100 mL/hr to the rate
- Limitation: Overestimates fluids 100 [Alvarado]
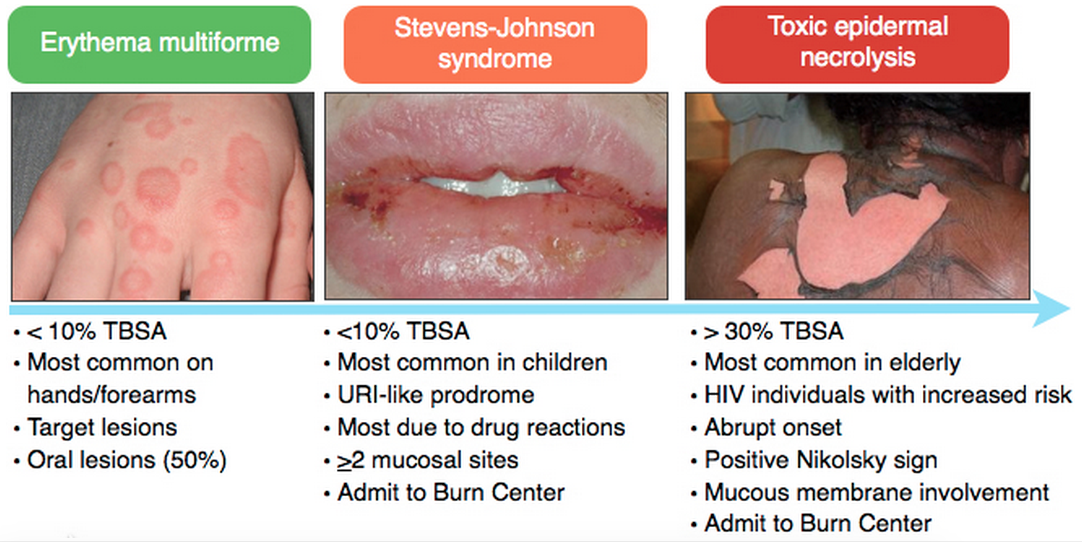
Consider Referral to Burn Center
Bad Burn –
- Partial thickness burns > 10% TBSA
- Full thickness burns
- Electrical burns or chemical burns
- Inhalation injury
Bad Place – Burns in the sensitive places such as face or genitals or important areas such as hands or major joints .
Bad Protoplasm – Preexisting medical disorders that could complicate management or prolong recovery (such as immunocompromised HIV patients).
Generously Donated Rosh Review Questions
Question 1. [polldaddy poll=8816037]
Question 2. A 52-year-old woman is brought to the emergency department with burns from a house fire. Physical exam reveals superficial burns over her entire left arm and partial-thickness and full-thickness burns covering her entire right arm, her anterior right leg and anterior trunk. [polldaddy poll=8824315]
Answers
1. C. Burn classification is based on burn depth. Second-degree burns are classified into superficial and deep partial-thickness burns. Deep partial-thickness burns extend into thereticular dermis. Skin color is usually a mixture of red and blanched white, and capillary refill is slow. Blisters are thick-walled and commonly ruptured and the skin may appear leathery white. Two-point discrimination may be diminished, but pressure and pinprick applied to the burned skin can be felt. Whereas superficial partial-thickness burns usually re-epithelialize 7-10 days after injury; so the risk of hypertrophic scarring is very small. For deep partial-thickness burns, tissue may undergo spontaneous epithelialization from the few viable epithelial appendages at this deepest layer of dermis and heal within 3-6 weeks. Because these burns have less capacity for re-epithelializing, a greater potential for hypertrophic scar formation exists. In deep partial-thickness burns, treatment with topical antimicrobial dressings is necessary to prevent infection as the burn wound heals. Contraction across joints, with resulting limitation in range of motion, is a common sequela. Splash scalds often cause second-degree burns.
2. B. The extent of burn size in this patient is 36% total body surface area. A thorough and accurate estimation of burn size is essential to guide therapy and to determine when to transfer a patient to a burn center. The extent of burns is expressed as the total percentage of body surface area. Superficial burns are not included in the burn assessment. For adult assessment, the most expeditious method to estimate total percentage of body surface area is the Rule of Nines. This method only takes into account partial-thickness and full-thickness burns. Each leg represents 18% total percentage of body surface area; each arm represents 9% total percentage of body surface area; the anterior and posterior trunk each represent 18% total percentage of body surface area; and the head represents 9% total percentage of body surface area. This patient has partial-thickness and full-thickness burns covering her entire right arm, her anterior right leg and anterior trunk, which calculates to 36%. The superficial burn on her left arm is not included in the calculation. According to the Rule of Nines, the percentage in this patient can be calculated as follows: entire right arm = 9%; anterior right leg = 9%; anterior trunk 18%. 9+9+18= 36%.

References:
1. Mlcak RP, Suman OE, Herndon DN. Respiratory management of inhalation injury. Burns. 2007;33:(1)2-13. [pubmed]
2. Kashefi NS, Nathan JI, Dissanaike S. Does a Nebulized Heparin/N-acetylcysteine Protocol Improve Outcomes in Adult Smoke Inhalation? Plast Reconstr Surg Glob Open. 2014;2:(6)e165. [pubmed]
3. Elsharnouby NM, Eid HE, Abou Elezz NF, Aboelatta YA. Heparin/N-acetylcysteine: an adjuvant in the management of burn inhalation injury: a study of different doses. J Crit Care. 2014;29:(1)182.e1-4. [pubmed]


 Indomethacin (B) is a non-steroidal anti-inflammatory agent commonly used in the treatment of acute gout. Gout is an arthritis caused by deposition of monosodium urate monohydrate crystals in the joint space. Acute flares involve a monoarticular arthritis with a red, hot, swollen and tender joint. Acute episodes of gout result from overproduction or decreased secretion of uric acid. However, measurement of serum uric acid (C) does not correlate with the presence of absence of an acute flare. A radiograph of the knee (D) may show chronic degenerative changes associated with gout but will not help to differentiate a gouty arthritis versus septic arthritis.
Indomethacin (B) is a non-steroidal anti-inflammatory agent commonly used in the treatment of acute gout. Gout is an arthritis caused by deposition of monosodium urate monohydrate crystals in the joint space. Acute flares involve a monoarticular arthritis with a red, hot, swollen and tender joint. Acute episodes of gout result from overproduction or decreased secretion of uric acid. However, measurement of serum uric acid (C) does not correlate with the presence of absence of an acute flare. A radiograph of the knee (D) may show chronic degenerative changes associated with gout but will not help to differentiate a gouty arthritis versus septic arthritis.